Practice Essentials
Worldwide, an estimated 152,863 solid organ transplants were performed in 2019. [1] In the United States, 39,000 organ transplantations were performed in 2020. [2] Renal transplants were the most common, followed by those of the liver, heart, lung, and others, including dual organ, pancreatic, and intestinal transplantation. Over the last several decades, the field of solid organ transplantation (SOT) science and practice has advanced significantly, only to be continually challenged by the risks for infection in SOT recipients.
The positive effects of the immunosuppressive agents, obligatory for the prevention of organ rejection, have been tempered by the negative effects of these same therapies, leading to various infections that range in both frequency and severity. [3] Fortunately, experienced SOT researchers and practitioners have been involved in the development and implementation of proactive guidelines such as the 2006 American Society of Transplantation guidelines [4] on screening, monitoring, and reporting of infectious complications in SOT recipients.
Newer immunomodulating agents have been developed, increasing the number of therapies that prevent organ rejection. However, this has simultaneously created newer unwanted opportunities for pathogens to cause infectious complications. [5, 6] These adverse effects are the result of their negative impact on both the cellular and humoral arms of the SOT recipient's immune system. Fortunately, newer diagnostic laboratory methods have also added much-needed capacity to identify the presence and types of pathogens, often early enough in the SOT recipient’s course to prevent or mitigate severe infection. [7]
Guidelines are constantly being refined to outline the most practical and appropriate screening processes to minimize donor-related infections. [8, 9, 10] Conversely, attention to implementing preventive measures such as pretransplant vaccination in SOT recipients also represents an important step in optimizing safe organ donation and retention. [11] Newer host-related challenges, such as the increasing prevalence of obesity, and system-related problems, such as healthcare-acquired infections, represent other challenges for successful infection prevention. [12, 13]
Finally, several areas related to infections in SOT recipients are unresolved and controversial. Recognized emerging issues include donor-derived infection (eg, arboviruses such as Zika, West Nile, and dengue; lymphocytic choriomeningitis virus [LCMV]) [14] ; drug-resistant infections, including multidrug-resistant tuberculosis; and many others; see webcasts from the 2016 International Transplant Infectious Disease conference here [account required]).
Given the broad scope of this topic and the availability of Medscape articles covering related areas in transplantation, the reader is referred to the relevant links available in the Medscape Transplantation volume. The September 2019 issue of the American Journal of Transplantation contains a comprehensive review of the various topics within the scope of infections in SOT recipients. [15] The focus of this article is adult populations, although infectious disease issues germane to the pediatric SOT recipient are discussed in Special Host Considerations.
Background Concepts
Immunocompromised hosts, regardless of underlying illness or factors leading to immunosuppression, commonly present diagnostic challenges in the face of severe infectious disease processes. These challenges are due to host factors that blunt or minimize symptoms and signs of inflammation. Medication toxicities compounded by allograft rejection and complications of healthcare-acquired infections result in more complex presentations.
As a result, practitioners are challenged to help solid organ transplantation (SOT) recipients retain their transplanted organs, prevent SOT-related infections, and improve their quality of life. The diagnosis of infection is made more arduous since SOT recipients may present with more than one infection or at later stages in the disease process or may experience drug toxicity from immunosuppressive agents, as well as from antibiotics. [16]
Transplant medicine is a discipline in which, perhaps more than any other field, practitioners must maintain a high index of suspicion for various complications and presentations. Clinicians must be astute and pay close attention to details related to epidemiologic clues, historical features, and physical signs. This helps in the often-difficult differentiation between infection and allograft rejection, which may present with similar symptoms, such as fever, cough, and diarrhea. [17, 18]
Although differentiating colonization from infection is often difficult in the clinical context, the clinician must exercise both prudence and vigilance in the approach to the febrile SOT recipient. Only then can a timely and accurate diagnosis be made while broad-spectrum empiric antimicrobial therapies are prescribed. [19] Primary care providers and specialists should maintain a low threshold of suspicion and promptly seek expert consultation when faced with a SOT recipient who presents with suspicion or evidence of infection, especially during the first several months posttransplantation.
Immunosuppressive Drugs Used in Solid Organ Transplantation
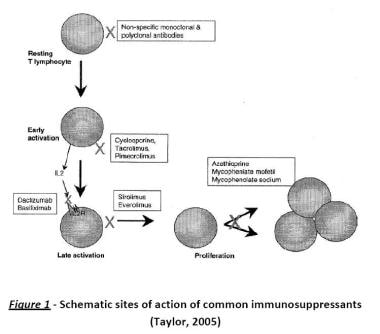
Although monographs on immunosuppressive drugs are available elsewhere in Medscape (see Immunosuppression), the information presented here relates to the specific mechanisms of drug action that underlie the specific types of immunodeficiencies predisposing to certain pathogens. [3, 20]
Immunosuppressive agents have the following 3 major effects:
-
The intended therapeutic effect of suppressing rejection
-
Deleterious acquired immunodeficiencies that the host sustains, leading to increased risk of infection or neoplasia
-
Direct or indirect toxicity to host tissues
Immunosuppressive agents used in transplantation target either single or multiple sites in the immune system, thus markedly enhancing their effect in prevention or treatment of organ rejection (via either single-drug or combination regimens). Therefore, these drugs represent a dual-edged sword, potentially predisposing solid organ transplantation (SOT) recipients to all categories of pathogens by impairing host defenses.
All of the major determinants of immune competence (host anatomic barriers, mechanisms in innate immunity, acquired capacities, presence or absence of immunomodulating co-infections, and underlying comorbid conditions) may be breached and may result in opportunistic pathogens, causing illness in SOT recipients. Examples of these factors include the following:
-
Immunosuppressive drug–induced antiproliferative activity leading to mucosal erosions
-
Transient cytopenias
-
Uremia
-
Hyperglycemia
-
Malnutrition
-
Use of invasive devices (leading to trauma, colonization, and infection)
-
Abnormalities in tissue perfusion (vascular or surgery-related etiologies)
-
Abscesses
-
Cytomegalovirus (CMV) infection
-
Epstein-Barr virus (EBV) infection
-
HIV infection
Given the complexity of variables that may positively or negatively affect immunosuppression in the SOT recipient, clear attribution of a particular pattern of immunosuppression to a specific immunosuppressive agent or regimen is difficult. Additionally, specific trends in the usage of various immunosuppressive therapies make it difficult to epidemiologically associate certain drugs with specific immunosuppression-related infections. Judgments on the likelihood of infection risks associated with specific drugs can often only be rendered based on minimal or suboptimal data on the infectious complications in immunosuppression drug trials. SOT recipients, like other immunocompromised hosts, often present with a mixture of immunological impairments, including neutropenia and lymphopenia, functional T-cell defects, lack of humoral antibody responses, and tissue damage. All of these add to the overall immunosuppression and predispose to infection with various pathogens.
Steroids
Corticosteroids and glucocorticoids constitute a major component of immunosuppressive medications used in SOT, often considered first-line therapy for allograft rejection. Agents such as prednisone or prednisolone have a myriad of negative effects on the immune system, including cell-mediated immunity impairment (through inhibition of several cytokines, including interleukin [IL]-1, IL-2, IL-3, IL-4, IL-5, IL-6, IL-8, and tumor necrosis factor [TNF]), often resulting in T-cell proliferation. Antigen presentation, through reduced expression of major histocompatibility complex molecules, also occurs. Humoral immunity is also suppressed, leading to the diminished production of IL-2 and related receptors, as well as B-cell clone expansion and decreased antibody synthesis.
Steroids induce a widespread decrease in the host inflammatory response, resulting in lipocortin-1 synthesis that can eventually impair migration of cells, phagocytosis, respiratory burst mechanisms, and the release of inflammatory chemokines and cytokines from white blood cells. Finally, apoptotic effects result in cytotoxicity. Clinically, these mechanisms of immunosuppression lead to an increased risk of bacterial, mycobacterial, viral, and fungal infections. Since 2000, steroid use appears to have decreased overall.
To better understand other groups of immunosuppressive drugs, a brief description of T-cell activation, which is a necessary step in immune responsiveness, is provided. To become activated, two signals are needed. The first signal, antigen-specific, occurs when peptide–major histocompatibility complex molecules interact with the T-cell receptor on the surface of antigen-presenting cells.
The second (costimulatory) signal does not depend on a specific antigen; it occurs when costimulator molecules are expressed on the antigen-presenting cell because of the interaction of the antigen-presenting cell with microbes. These costimulators are recognized by the CD28 receptor on the T cells, resulting in further T-cell proliferation and differentiation.
Other immunosuppressive agents
In addition to steroids, the following classes of immunosuppressive agents are of clinical significance:
-
Small-molecule drugs, including antiproliferative drugs (eg, azathioprine, mycophenolate mofetil, mycophenolate sodium)
-
Calcineurin inhibitors (eg, cyclosporine, tacrolimus)
-
Inhibitors of mammalian target of rapamycin (mTOR) (eg, sirolimus, everolimus)
-
Protein drugs (polyclonal antilymphocyte antibodies and monoclonal antibodies)
Examples of polyclonal antibodies (targeted against lymphocytes) include antilymphocyte globulin (ALG) and antithymocyte globulin (ATG). Examples of monoclonal antibodies include muromonab-CD3 and basiliximab.
The image below shows the schematic sites of action for some of these common agents.
Antiproliferative drugs
Azathioprine primarily targets enzymes in the de novo synthesis of purines, leading to the impairment of DNA replication in dividing cells, such as lymphocytes. Therefore, while sparing any cytotoxic effects on T cells prior to an antigen challenge, activated T cells are the main target. Marked immunosuppressive effects occur after antigen stimulation; B cells are also immunosuppressed. As a result of all of these effects, patients receiving azathioprine may experience bone marrow suppression, gastrointestinal intolerance, and infections. Patients who are receiving azathioprine tend to develop major viral infections (such as with herpes viruses), as well as fungal and parasitic infections.
Mycophenolate mofetil is the prodrug of mycophenolic acid. Administration of this drug ultimately causes inhibition of the enzyme inosine monophosphate dehydrogenase, which is involved in the de-novo synthesis of guanosine nucleotides. The immunosuppressive effect tends to be selective for B and T cells, mainly decreasing the proliferation of activated T cells. Since humoral responses can also be impaired, immunization practices will not likely be effective, especially if vaccine is given during mycophenolate mofetil therapy.
The infectious complications of mycophenolate mofetil administration are similar to those associated with azathioprine; the increased CMV risk in patients receiving mycophenolate mofetil is not easily explained. Ironically, mycophenolate mofetil protects against infection due to Pneumocystisjiroveci.
Calcineurin inhibitors and mTOR inhibitors
These two classes of drugs belong to a group of agents that bind to immunophilins, which are immunosuppressant binding proteins involved in lymphocyte activation. The calcineurin inhibitor–immunophilin complexes block the function of the enzyme calcineurin at different enzymatic sites, resulting in the blockade of normal calcineurin dephosphorylation activity that involves the cytoplasmic component of the nuclear factor of activated T-cells (NFAT). This prevents NFAT from binding to the nuclear component of NFAT, which, under normal circumstances, binds to the promoter of the IL2 gene. [21] The end result is that the calcineurin inhibitors impair the T-cell synthesis of IL-2.
One study looked at 410 liver transplant recipients who were treated with pegylated interferon and ribavirin for recurrent hepatitis C viral infection. Multivariate analysis showed that a higher sustained virological response (SVR) correlated with cyclosporine-based immunosuppression regimens (odds ratio [OR], 0.37; P = 0.021) in conjunction with a longer antiviral treatment duration (OR, 0.86; P = 0.024). The authors do note that this data should be further confirmed in prospective clinical trials. [22]
Cyclosporine administration increases the risk of posttransplant lymphoproliferative disorder (PTLD), an EBV-associated condition. An important difference between cyclosporine and tacrolimus is that the latter is far more potent than cyclosporine and broader in its inhibitory effect on other transcriptional factors, resulting in decreased production of not only interleukin-2 (IL-2) but also IL-3, IL-4, IL-5, interferon (IFN)–gamma, and other cytokines. The trend is for greater substitution of cyclosporine with tacrolimus in the maintenance phase of immunosuppression.
Conversely, the mTOR inhibitor agent sirolimus (or rapamycin), a macrolide antibiotic, binds to its respective binding protein, mTOR, in the cytosol, inhibiting normal biochemical pathways needed for mRNA translation critical for cell division. In contrast to calcineurin inhibitors, which decrease IL-2 levels, the mTOR agents block cytokine signal transduction for T- and B-cell activation. The mTOR inhibitors also inhibit fibroblast growth factors, which may result in wound-healing problems. Although sirolimus has been noted in studies to enable cyclosporine withdrawal posttransplantation, it can also induce an inflammatory reaction, resulting in an atypical pneumonia–like picture or leukoencephalopathy. This mimicry may present significant diagnostic challenges.
Since the calcineurin inhibitors are often used in combination with other classes of immunosuppressive therapies, [23] their specific clinical effects on host immunity are difficult to ascertain. Infections from two pathogens, CMV and polyoma BK virus, appear to be directly related to the immunosuppressive effects of the calcineurin inhibitors. [23]
Cyclosporine has been reported to suppress the replication of hepatitis C virus (HCV) and increase sustained virological response after transplantation, an effect that was not detected with tacrolimus. However, a meta-analysis and systematic review by Liu et al found no significant difference between tacrolimus-based and cyclosporine-based immunosuppression with regard to posttransplant mortality from HCV recurrence, graft loss, and retransplantation, as well as histological HCV recurrence. [24]
Antibodies
The class of polyclonal antibodies (eg, antithymocyte globulin, antilymphocyte globulin) has traditionally been used in the induction phase of immunosuppression. Although induction therapy in the field of transplantation has increased since the mid 1990s, antithymocyte globulin has largely replaced the use of antilymphocyte globulin and monoclonal antibodies such as muromonab-CD3 (OKT3).
Although OKT3 was once widely used and is still used in specific rejection syndromes, it has unfortunately been associated with the toxic cytokine release syndrome, which is due to a massive activation of T cells and consequent clinical effects such as pulmonary edema, aseptic meningitis, and graft thrombosis. This widespread activation results from the binding of OKT3 to its target surface antigen, CD3 receptor, a membrane protein located on T-lymphocyte cell surfaces.
With respect to antithymocyte globulin use and subsequent infection in the SOT recipient, the impact on bacterial infections overall may be potentially confounded by other factors, including the effect of postoperative complications, presence of invasive devices, and use of other immunosuppressive agents. Antithymocyte globulin increases the risk for CMV infection, as well as for BK virus viremia and nephropathy. Infections with Pneumocystis species and other invasive fungal pathogens have been associated with antithymocyte globulin therapy.
Other types of monoclonal antibodies have been developed, including ones that target the alpha chain of the IL-2 receptor (IL-2R), named anti-CD25 antibody. Such agents interfere with the initial expansion of T cells following antigen-specific stimulation. Anti-CD25 agents (eg, basiliximab) are used in induction therapy and are supported by studies that have shown a decrease in infection rates compared with the use of antithymocyte globulin; they may also allow doses of concurrently used immunosuppressive therapies to be reduced.
These drugs do not usually lead to a sustained depletion of lymphocytes and related CD4 helper T cells, unlike the depletion seen with alemtuzumab (another monoclonal antibody directed against CD-52). However, when all of these agents are used for an extended period, increased rates of severe infection have been observed, even long after the transplantation was performed. Generally, IL-2R antagonists have not been associated with an incidence of bacterial infections greater than that associated with other induction therapies or placebo. The incidence of CMV, EBV (and EBV-induced PTLD), and fungal infections with these antagonists has been similar to that seen with other induction regimens. However, patients undergoing T-cell depletion induction are at greatest risk for most CMV-associated complications.
The effect of IL-2R antagonists on hepatitis C infection is unknown. Alemtuzumab can essentially result in pan–T-cell depletion; counts of CD4 and CD8 cells can reach their lowest points 4 weeks after initiation of therapy. This agent appears to be more associated with opportunistic infections, including viral infections (herpes simplex virus in particular), although all of the monoclonal antibody products likely contribute to immunosuppression to a degree that places the SOT recipient at risk for various pathogens.
Investigational agents
Several new agents, some of which are in phase II and III trials, include the following:
-
Leflunomide, an antiproliferative agent similar to methotrexate (approved for use in rheumatoid arthritis)
-
Belatacept, a costimulatory blocker that has been associated with some cases of PTLD (which may limit the drug's use if future data confirm an adverse relationship)
-
Agents that target adhesion and transmigration
-
Efalizumab, another type of monoclonal antibody
-
Fingolimod, a sphingosine-1-phosphate receptor 1 modulator (approved for use in multiple sclerosis)
The advent of these types of therapies may signal a shift toward more specific and targeted approaches to the prevention and treatment of transplant-related rejection. This paradigm, which also includes newer developments in study design, better monitoring of infectious complications, and newer diagnostic methods that enable tailoring of therapies to SOT recipients, will hopefully enable even greater reduction of SOT-related infections.
Statins
Statins have demonstrated their ability to improve outcomes in patients with cardiovascular disease, including those with a history of transient ischemic attack, cerebrovascular accident, carotid artery stenosis, coronary restenosis, and cardiac dysrhythmias. In patients with chronic kidney disease, statins have significantly reduced fatal and nonfatal cardiovascular events.
Notwithstanding legitimate concerns about adverse drug interactions between statins and cyclosporine, increasing the risk of rhabdomyolysis in solid organ transplantation (SOT) recipients, the prevalence of metabolic complications posttransplantation that may respond to statins has led to an increase in their overall use. Clinical studies are still needed to confirm their overall benefit in this patient population.
Multiple studies have shown that other statin-induced effects may have significance in SOT recipients. Statins can attenuate the virulence and pathogenicity of organisms. These drugs also have immunomodulatory effects on cell signaling and regulatory pathways related to pathogenesis and control of various infections. [25] Indeed, statins have demonstrated protective antimicrobial effects against several organisms, including bacteria such as Staphylococcus aureus and Mycobacterium tuberculosis; viruses such as BK virus, CMV, EBV, and hepatitis C; and fungi such as candidal species, cryptococcal species, and invasive species (Aspergillus and Zygomycetes).
Broadly, as a result of their anti-inflammatory actions, statins have decreased hospitalization rates in patients with sepsis on dialysis and the risk of pneumonia in patients with diabetes. The exact mechanisms involved in statin-related modulation of the inflammatory response in sepsis have yet to be determined but are likely to involve statin-induced alteration of cytokine, chemokine, adhesion molecules, and cellular immune function.
Timeframe
Net state of immunosuppression
The concept of the "net state of immunosuppression" [26, 27] has been pivotal to the understanding of not only solid organ transplantation (SOT) but also bone marrow transplantation–related infectious disease complications. Admittedly, many variables can potentially contribute to the development of infections in the SOT recipient. These factors exist within the domains of the SOT recipient's health, nutrition and host immunodeficiencies, immunosuppressive drug regimens, healthcare institutions, donor-derived organ-related infections, and the presence or absence of comodulating viruses.
All of these may positively or negatively affect the overall risk of infection. It is the net effect of the confluence of any and all such relevant factors in any given SOT recipient that ultimately determines the incidence, timing, and severity of infection. Since these influential variables dynamically interact to create the net state of immunosuppression, it is not a fixed phenomenon but represents a fluid process. [26]
This requires vigilance and proactivity of clinicians as they help SOT recipients navigate through the pretransplant, operation, and posttransplant phases. This net state of immunosuppression is also a function of time, since periods following transplantation during which certain types of infections and pathogens may present with greater probability are fairly well defined. Importantly, once a SOT recipient undergoes acute rejection, requiring treatment interventions, it tends to set back the clock to the period when transplantation occurred and the initial postoperative immunosuppression began. [26]
Timeframes around transplant-related infections
For almost 2 decades, clinicians caring for SOT recipients have been able to guide infection-prevention and control management strategies based on the classic timetable originally proposed by Rubin et al. Although newer immunosuppressive and antimicrobial prophylactic regimens have affected the pattern and timing of specific infections posttransplantation, certain general observations still hold true. Some variance may be considered according to the type of organ transplanted. Initial infection risk stratification is a process determined by factors such as donor and recipient screening status, operative and perioperative outcomes, and the degree of immunosuppression and other factors (discussed below). [27]
One of the most important consequences of an episode of organ rejection or increased immunosuppression (from regimen modifications) is that the overall timeframe tends to get reset to an initial period of vulnerability comparable to the transplantation itself. Over the subsequent 6 months posttransplantation, 3 periods provide a structural approach to the infectious disease management (see image below).
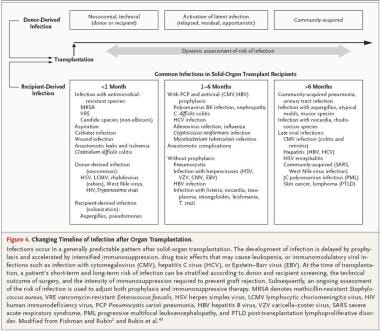 Changing timeline of infection after organ transplantation (modified from Fishman J. NEJM. 2007;357(25):2601-14).
Changing timeline of infection after organ transplantation (modified from Fishman J. NEJM. 2007;357(25):2601-14).
Within the first 30 days after transplantation, the patient is at greatest risk for healthcare-associated infections, often due to antibiotic-resistant organisms and often polymicrobial in etiology. [26]
These infections, as is the case for healthcare-acquired infections in general, are often procedure- or device-related, such as catheter-associated infections (urinary tract, bloodstream infections), ventilator-associated pneumonia, aspiration, surgical wound infections, or are associated with anastomotic leaks and ischemia. Unfortunately, infections may also result from modification of endogenous microbial flora in the recipient or extant or new colonization (often related to the healthcare environment, including the hands of healthcare workers), such as with Clostridium difficile and its spore-induced toxins.
Superinfections may even develop, and these may carry a poor prognosis. Specific organisms across the range of pathogen categories (ie, opportunistic viruses, bacteria, fungi, and parasites derived from the donor, recipient, or both) may cause infection during this first month. Overall, the types of infection during this period share patterns with those that routinely occur after similar operations.
The second period (approximately 1-6 months posttransplantation) is characterized by the presence or absence of those pathogens selected for by whether or not there are ongoing prophylactic antibiotics against P jiroveci or viruses such as CMV or hepatitis B. [26, 28] The preventive antimicrobial agents used for these organisms also have efficacy against other opportunistic pathogens, such as common bacteria, Listeria, Nocardia, Strongyloides, and herpesviruses such as herpes simplex virus, [29] varicella-zoster virus, [30] and EBV. Importantly, concurrent CMV infection during these 5 months may have an independent immunosuppressive effect, placing SOT recipients at risk for opportunistic organisms and contributing to almost two thirds of febrile episodes during this period.
CMV infection/illness may manifest as systemic symptoms such as fever, arthralgias, myalgias, or organ-specific symptoms.
After 6 months, patients fall into the following three groups:
Eighty percent have adequate allograft functioning (and minimal immunosuppression characterized by the absence of chronic viral infection)
Approximately 15% have chronic viral infections.
About 10% have frequent rejection episodes, immunosuppression due to treatment regimens, infections with viruses such as CMV, or a combination of these.
Infections most commonly found in the first group include community-acquired viral infections (eg, influenza, parainfluenza, respiratory syncytial virus, human metapneumovirus), bacterial infections (eg, Streptococcus pneumoniae, Haemophilus influenzae), urinary tract infections, and asymptomatic cryptococcal infection (eg, asymptomatic pulmonary nodules).
The second group is at special risk for infections with adenovirus, polyomavirus BK, recurrent hepatitis C, human papillomavirus (HPV), and HIV. Chronic viral infections may also lead to different types of allograft dysfunction.
The third group often presents with severe opportunistic infections involving P jiroveci, Cryptococcus neoformans, Nocardia, Rhodococcus, and invasive fungi such as Aspergillus, Mucor, and other molds. [31, 32]
Finally, malignant neoplastic diseases that originate from or are modulated through infectious organisms can develop during periods of immunosuppression, albeit in the later posttransplantation period. Examples include the following:
Framework for Infection Risk Assessment
Remaining vigilant to the concept of net state of immunosuppression, the clinician is advised to approach solid organ transplantation (SOT)–related infections using a framework of infection risk assessment based on exposure to organisms potentially acquired through the following six different paths [26] :
-
Community-acquired pathogens
-
Reactivation of previous infections (either from donor or recipient)
-
Specific epidemiologic exposures, including hobbies, food and water, work, recreational activities, pets, zoonotic infections, or sexual activity [27]
-
Infection specific to the donor organ
-
Iatrogenic or healthcare-associated infections
-
Specific travel-associated pathogens, including a range of tropical diseases
This framework will hopefully enable the clinician to relate organism category (bacteria, viruses, fungi, parasites) to each of these 6 potential sources of exposure and infection. The framework for infection risk assessment in the solid organ transplant recipient is discussed below, with CREDIT used as a mnemonic device, as follows:
-
C – Community acquired
-
R – Reactivation
-
E – Epidemiologic exposure
-
D – Donor derived
-
I – Iatrogenic
-
T –Travel related
Community-acquired infections
Community-acquired infections are common and include colds, viral and bacterial lower respiratory infections, and gastrointestinal infections. With the increasing complexity of epidemiologic patterns affecting communities, pathogens such as methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant Streptococcus pneumoniae may also fall into this general group.
Atypical organisms such as Mycoplasma, Legionella, and Chlamydia species, as well as prevalent vaccine-preventable diseases, may also cause disease in SOT recipients. Specific viral pathogens include the following:
-
Influenza viruses
-
Parainfluenza viruses
-
Respiratory syncytial virus
-
Adenovirus
-
Human metapneumovirus
-
Rhinoviruses
-
Coronaviruses
Reactivation
Donor-specific reactivation-related disease is largely mediated through transmission via the donated organ. Organisms that can lead to clinical infection and even endogenous immunosuppression (eg, CMV) from a process of reactivation within the SOT recipient include the following:
-
M tuberculosis
-
Atypical mycobacteria
-
Parasites ( Strongyloides stercoralis, Trypanosoma cruzii, Leishmania species)
-
Herpesviridae (CMV, EBV, herpes simplex virus, varicella-zoster virus)
-
Other viruses (HIV, hepatitis B, hepatitis C, papillomavirus, BK virus)
-
Endemic fungi ( Histoplasma capsulatum, Coccidioides immitis, Paracoccidioides brasiliensis)
Epidemiologic exposure
Realizing that accurate and timely assessment of the SOT recipient's risk of infection is directly related to his or her involvement in specific activities may be of great epidemiologic significance in the evaluation of the febrile SOT recipient. In fact, such an assessment is of importance on a preventive basis, since proactive identification of epidemiologic exposure that increases the SOT recipient's risk may represent a cost-effective way to mitigate against infection in the first place. [35] This kind of history-taking is especially important in the context of immunosuppression, since infection and ultimate disease may depend on the dynamic interaction between specific exposures and specific immune deficits (eg, anatomic, cellular-immunity, humoral, complement).
Based on a standard approach in the evaluation of fever of unknown origin or febrile illness in any immunocompromised host, clinicians are encouraged to fully explore the following areas for epidemiologic clues:
-
Place of birth (eg, foreign-born)
-
Prior/recent domicile (eg, homelessness)
-
Employment status and workplace conditions
-
Recreational habits (eg, alcohol, cigarettes, recreational drugs [including intravenous drugs])
-
Hobbies (eg, water sports, gardening, bird-watching)
-
Transfusion history
-
Incarceration history
-
Sexual history (eg, current/former partners, barrier precautions, history of prior sexually transmitted diseases)
-
Potential exposure to arthropod vectors (eg, spelunking, hiking)
-
Pets (eg, dogs and cats [recent/remote bites], kittens [catscratch disease], reptiles [enteric infections], birds [eg, psittacine exposures], exotic animals, including sources of acquisition)
-
Current medications (eg, antacids, protein-pump inhibitors with risk of achlorhydria)
-
Food or water exposures (potential for food-borne organisms/toxins)
-
Comorbid illness that increases the risk of infection (eg, diabetes [36] , chronic lung disease)
Donor-derived infections
Donor-derived infections are of particular significance, as evidenced by several reports of infectious diseases transmitted through transplanted organs. They include viruses (hepatitis B and C, [37] herpes viruses, human T-cell lymphotropic viruses (HTLV) 1 and 2, West Nile virus, rabies, LCMV, polyomavirus BK/JC, HPV, parvovirus B19, HIV), mycobacteria (tuberculous and nontuberculous mycobacteria), meningococcus, syphilis, parasites (malaria, Babesia, Toxoplasma gondii, Trypanosoma cruzi [Chagas disease], S stercoralis), and several fungal organisms. Donor-derived drug-resistant bacteria may also be transmitted, including vancomycin-resistant enterococci, MRSA, and fluconazole-resistant Candida species. [38]
Iatrogenic considerations
Invigorated efforts toward increasing patient safety, minimizing errors, and increasing adherence to hand hygiene reinforce the vigilance required of healthcare workers and patients in their efforts to mitigate the risk of acquiring iatrogenic or healthcare-acquired infections. As noted above, specific patterns of infection exist, especially in the first month after transplantation, that are also carried forward throughout all phases in the natural posttransplant history whenever the SOT recipient interfaces with the healthcare setting.
Travel considerations
Attention to recent and remote travel is an important component of infection risk assessment. [39] There are many emerging and re-emerging infectious diseases across a range of pathogen categories. Some important pathogens in this category of exposure include the following:
-
Escherichia coli (eg, enterotoxigenic E coli)
-
Mycobacterium leprae (leprosy)
-
HTLV 1 and 2
-
Penicillium marneffei
-
Plasmodium species
-
Filarial species
-
Echinococcus species
-
Schistosoma species
-
Clonorchis species
-
Trypanosoma brucei
-
Taenia solium
-
Entamoeba histolytica.
Kotton et al [40] and Franco-Paredes et al [41] have published excellent reviews on prevention of infection in travelers after SOT. Trubiano et al have published a guide to travel vaccination recommendations and endemic pathogen risks for SOT recipients. [42] The exhaustive compilation of tropical and geographically restricted infections during SOT by Martin-Davila et al [43] is also an excellent resource.
Selected Pathogens of Clinical Significance in Solid Organ Transplant Recipients
Many opportunistic pathogens have been reported in solid organ transplantation (SOT) recipients, resulting in a wide variety of organ-based pathology or septic syndromes. Briefly mentioned in this section are some highlights on the epidemiology and diseases related to bacterial, viral, and fungal organisms of special significance (because of an increased incidence, greater virulence, or prototypic role in the SOT recipient). Parasitic disease is not discussed, but the reader is referred to a review by Coster. [44]
Bacterial infections
Among bacterial pathogens, infection with antibiotic-resistant bacteria that include MRSA, vancomycin-resistant enterococci, and Clostridium difficile, along with gram-negative healthcare-associated bacteria, play a significant role, especially in the postoperative period (< 30 days posttransplant). [45, 46, 47] For example, studies have shown that SOT recipients are at higher risk of multidrug-resistant Pseudomonas aeruginosa bloodstream infection, which carries a high mortality rate. [48]
Conversely, although some studies have shown no difference in the severity of C difficile–associated diarrhea (CDAD) in SOT recipients compared with non-SOT recipients, exposure to steroids placed SOT recipients at a significantly higher risk of relapse, often requiring a longer course of CDAD therapy. [13, 49] A 2012 study, which defined complicated clostridium difficile colitis (CCDC) as CDAD associated with graft loss, total colectomy, or death,showed the peak frequency of CDAD to be between 6 and 10 days posttransplantation. Independent risk factors for CDAD included age greater than 55, induction with antithymocyte globulin, and transplant other than kidney alone (liver, heart, pancreas, or combined kidney organ). Predictors of CCDC were white blood cell count >25,000/µL and evidence of pancolitis on computed tomography scan. Colectomy was done with excellent survival (83%) in some patients. [50]
Opportunistic pathogens such as Legionella remain a major challenge in SOT recipients. Microaspiration of water or inhalation of aerosols contaminated with Legionella can result in outbreaks in transplant centers similar to other healthcare settings. The 2- to 6-month period following SOT is the critical time when these infections are generally seen, although community-acquired Legionella infection can occur any time.
Listeria monocytogenes is yet another pathogen resulting in bacteremia, meningitis, and sepsis following SOT, often months to years after the surgery. Other organ manifestations of Listeria infections include endocarditis, endophthalmitis, brain abscess, and infections of allograft sites (eg, liver, heart).
Nocardia infections may present in a localized or disseminated pattern. Nocardia are aerobic bacteria that stain weakly acid-fast with the appearance of beaded, branching, thin filaments. [51] These organisms are generally inhaled, establishing a pulmonary infection that may result in pneumonia or cavitary lesions, followed by dissemination to brain, bone, or skin. Although relatively rare in SOT recipients, Nocardia infections may be particularly challenging because of their subtle presentations and fastidious nature. [52] A matched case-control 5-year study found that independent risk factors for Nocardia infection among SOT recipients include history of high-dose steroids, CMV disease, and use of calcineurin inhibitors. Intestinal SOT recipients may be at increased risk for nocardiosis.
A particularly challenging pathogen is M tuberculosis. [53] Most tuberculosis-related illnesses in the SOT recipient are caused by reactivation of tuberculosis in the recipient in the context of transplantation-related immunosuppression. [54, 55] Only approximately 4% of tuberculous infections in recipients are donor-transmitted. [56]
Data from European centers indicate a 9.5% attributable mortality rate in SOT recipients who develop clinical tuberculosis, with age and lung transplantation being independent risk factors. [57, 58] Particularly important issues include (1) the higher prevalence of atypical presentations, including extrapulmonary tuberculosis and disseminated disease among SOT recipients; (2) the critical need to identify and treat latent tuberculosis; and (3) management of pharmacological toxicity and drug interactions between tuberculosis therapies and SOT-related medications. [59] Drug-resistant tuberculosis can be particularly important in SOT recipients, given the challenges of such disease in an immunocompromised host. [60]
The association between Helicobacter pylori and gastrointestinal disease (eg, peptic ulcer disease, chronic gastritis, gastric adenocarcinoma, mucosa-associated lymphatic tissue lymphoma) is well known. The prevalence of H pylori appears to be similar between SOT and nontransplant patients but tends to decrease after transplantation, likely because of the significant impact of post-SOT antimicrobial therapy. [61] The incidence of H pylori –related complications does not appear to increase in the post-SOT phase; however post-SOT management should still include surveillance and monitoring for these complications and prompt preemptive interventions for H pylori.
Therefore, eradication strategies for H pylori, though not completely evaluated thus far, should be implemented in the context of risk factors and/or symptomatology. An important confounding variable is the variety of gastrointestinal toxicities caused by existing immunosuppressive therapies (eg, calcineurin inhibitors, mycophenolate mofetil, steroids). [62]
Viral infections
Many viruses associated with SOT lead to opportunistic illness. These include CMV, EBV (and PTLD), and BK virus, as well as viruses previously considered less significant in SOT, such as hepatitis E. [63, 64, 65, 66] Emerging pathogens such as arenaviruses are associated with fatalities. [67]
CMV is the most important viral pathogen to consider in SOT recipients. More than half of SOT recipients develop CMV infection within the first 3 months after transplantation; however, like other pathogens, CMV can also cause illness in later phases. [68] The general prevalence of CMV seropositivity is 80%-90%, with most primary infections occurring in childhood or adolescence. Latent infection reservoirs include the reticuloendothelial system, peripheral lymphocytes, and monocytes, resulting in later reactivation in the context of immunosuppressive therapies. Well-designed studies have shown that patients treated with sirolimus have a lower incidence of CMV infection. Those patients likely received induction therapy with T-cell depletion. [69]
However, CMV infection can result from allograft infection, blood products, or natural infection posttransplantation among CMV-negative SOT recipients. Besides nonspecific febrile presentations, CMV can result in invasive disease and organ dysfunction. [70, 64, 71]
Of note, it is still unclear why CMV does not usually present with retinitis syndromes in SOT recipients, unlike in individuals with advanced HIV/AIDS in whom cellular immune dysfunction is also very prevalent. [72] Copathogens, including HHV-6 or HHV-7 viruses and P jiroveci, may lead to complicated severe disease patterns. [73, 74] CMV, because of its immunomodulatory effects, may compound existing immunosuppression, causing secondary infections with bacteria and fungi. A meta-analysis of 16 studies found post-transplant CMV disease/syndrome significantly increased the risk for development of invasive aspergillosis while asymptomatic CMV viremia/infection did not. [75]
Prompt and effective management of chronic rejection associated with CMV infection needs to be a priority. Chronic allograft rejection may lead to various syndromes, including vanishing bile duct syndrome, bronchiolitis obliterans, coronary atherosclerosis, and nephropathy in recipients of liver, lung, heart, and kidney transplantation, respectively. CMV also has indirect effects, such as the secondary onset of diabetes after CMV infection in SOT recipients. Finally, superinfection can also lead to serious consequences, eg, transmission and reactivation of donor-derived CMV in a seropositive recipient. [76]
Specific diagnostic and treatment recommendations regarding CMV are available in Medscape’s Cytomegalovirus article. A review by Kotton et al offers international consensus guidance on the management of CMV infection in SOT recipients. [77]
However, note that resistance has been noted against valganciclovir (VGCV), resulting from UL97 and UL54 gene mutations. In one study, the incidence and outcomes of ganciclovir-resistant CMV viremia was investigated in 1244 patients. The investigators’ dosage for preemptive CMV treatment (VGCV 900 mg/d) was associated with a high incidence of CMV UL97 -resistance gene mutations. After reducing the effected patients’ immunosuppressive therapy, foscarnet was given to some of the patients, which rapidly and safely cleared the virus; those not given foscarnet continued on VGCV treatment andeventually cleared the virus. [78]
EBV infection is also extremely prevalent, with almost 95% of the population being infected (often asymptomatically) by adulthood. Notwithstanding the common infectious mononucleosis syndrome, it was noted decades ago that EBV can be cultured from Burkitt lymphoma cells. EBV can remain latent in B cells and chronically replicate in oropharyngeal tissue. Although multiple viral genes are expressed in the life cycle of EBV infection, the presence of EBV DNA through EBV nuclear antigen and EBV latent membrane protein can be detected in tissues characteristic of PTLD. In reviews of PTLD from the 1990s, the average time for PTLD to manifest was around 32 months post-SOT. PTLD tended to develop much more quickly (< 6 mo) in patients receiving cyclosporine. [79]
The frequency of PTLD varied by type of organ transplantation, from approximately 2% in kidney and liver transplants to 4.9%-13% in cardiac transplants (likely due to the greater degree of needed immunosuppression). Some of the clinical presentations of PTLD include nonspecific febrile illness, mononucleosislike illness, gastrointestinal bleeding, infiltrative allograft involvement, and CNS disease. PTLD tumors tend to be aggressive and, although treatments are available, are often associated with poor outcomes (in part due to the complexity of presentations). See the Medscape article Posttransplant Lymphoproliferative Disease for more information.
Another significant viral pathogen, BK virus, has been a particular challenge in the context of kidney transplantation. [80] Part of the Papovaviridae family of viruses, BK virus was in fact named after it was initially detected in the urine of a kidney transplant recipient whose initials were BK. The primary infection is often asymptomatic and is likely spread from person to person and associated with dissemination to the kidneys, where it may remain latent. [66] Up to 20%-40% of SOT recipients may have viruria, with approximately 12% presenting with actual viremia. The clinical presentation largely involves the development of polyomavirus-associated nephropathy. Although multiple risk factors are associated with this condition, the two main necessary elements are the coexistence of viral infection and intensified immunosuppressive regimens that include, for example, tacrolimus, mycophenolate mofetil, and prednisolone. [81]
Although reduction of immunosuppression is warranted as an effort to improve the immunologic response against infection with BK virus, cautious antirejection treatment in patients with active BKV infection can result in a lack of clinical response, which, in turn, makes it challenging to differentiate refractory rejection from viral-induced inflammatory changes in the tissue. [20] Although viral load assays of BK virus DNA (polymerase chain reaction [PCR]) in the context of progressive renal dysfunction can help with diagnosis, definitive diagnosis is based on positive renal allograft biopsy results (at least 2 core biopsy specimens, ideally sampling the renal medulla, where virus is more likely present) and positive immunohistochemistry tests using antibodies against BK virus or cross-reacting SV40 large T-antigen. [82, 83] Cidofovir, at low doses, is an effective agent for treating polyomavirus-associated nephropathy, despite having known nephrotoxic effects.
Although it is not discussed in further detail in this article, an important virus that can cause primary disease or act as a copathogen is adenovirus, which has been associated with hemorrhagic cystitis. It is diagnosed with the aid of culture or antigen detection/immunofluorescence. [84, 85, 86]
Chronic infection with hepatitis E virus, an RNA virus similar to the Caliciviridae family (which includes norovirus), may occur in SOT recipients. [65] Hepatitis E virus is transmitted via the oral-fecal route and is known to primarily cause acute hepatitis, often with a fulminating course in certain hosts such as third-trimester pregnant women. In industrialized countries, hepatitis E virus tends to have a zoonotic pattern, with pigs, cattle, sheep, ducks, goats, and rats known to be infected. [87]
SOT recipients with liver, kidney, and kidney-pancreas transplants can develop chronic hepatitis E infection, and viral RNA levels can persist for a median of 15 months after the acute phase of illness is over. Histologic findings in patients with chronic hepatitis C infection have included lymphocytic portal infiltrates with piecemeal necrosis. [65] SOT recipients with chronic hepatitis E infection were noted to have lower total lymphocyte counts, as well as specific T-cell subsets, including CD2, CD3, and CD4. Seroconversion of hepatitis E virus occurred later in SOT recipients with chronic hepatitis than those whose acute infections resolved. [65]
The use of intense immunosuppressive regimens including mycophenolate mofetil and/or mTOR inhibitors appeared to be risk factors for chronic hepatitis E viral infection development and progression. In fact, chronic hepatitis E infection in a renal transplant recipient was reported to rapidly progress to cirrhosis. This particular case was noted also for the lack of hepatitis E immunoglobulin G seroconversion, which, in light of a prior positive immunoglobulin M level (and recurrently elevated hepatitis E virus RNA in the chronic active hepatitis phase of illness), became a false-negative finding, likely because of the patient’s immunosuppressed condition.
In a study of 59 SOT recipients with chronic hepatitis E infection, Kamar et al reported that ribavirin as monotherapy may be effective. A 3-month course seemed to be an appropriate duration of therapy for most patients.
Arenaviridae are enveloped RNA viruses most often implicated in rodent-human transmissions from exposure to infected urine. Infection with the most characteristic arenavirus, LCMV, may be asymptomatic or may be associated with mild illness but can also lead to aseptic meningitis or encephalitis; however, most people recover without complications. [67]
A new arenavirus was reported to be associated with a cluster of fatal cases in which three SOT recipients (two kidney and one liver recipient) developed a rapidly progressive febrile illness several weeks after transplantation. [67] All 3 patients were linked to a single donor, and all died within a few days of one another; diagnosis was made efficiently using newer molecular techniques including unbiased high-throughput sequencing, with later specificity of sequences being confirmed by culture and other tests.
Fungal infections
Among fungal pathogens, the most common opportunistic fungi include Candida species, molds such as Aspergillus, and cryptococci. [88, 89, 90, 91] Endemic geographically limited systemic mycoses, including coccidioidomycosis, blastomycosis, and histoplasmosis, can cause significant illness in the SOT recipient. [92] Endemic fungal infections may manifest as primary rapidly progressive syndromes with hematogenous dissemination to various organs; in recipients, reactivation infection followed by further spread and re-infection in the context of transplant-related immunosuppression may also occur.
Emerging pathogens, such as Fusarium, Scedosporium, and Trichosporon species, can cause various syndromes [93] that are similar to those caused by Aspergillus species, which also have a vascular predilection, causing invasive disease complicated by hemorrhage and infarction. [94, 95] Many patients already have metastatic site involvement at the time of presentation, which is associated with high mortality rates—often up to 50% despite intravenous therapy. [96]
Candida species, the most common fungal pathogens, are associated with a range of presentations, including milder albeit painful forms such as thrush, mucositis, and asymptomatic candiduria. Severe disease with organ involvement is also possible, with manifestations such as hepatosplenic candidiasis, endocarditis, and genitourinary syndromes. Candidal infection presenting as bloodstream infection may also be associated with healthcare settings, especially with the use of invasive devices.
Fortunately, because of many factors, including greater use of prophylactic regimens, advanced surgical methods, and modifications in SOT immunosuppressive regimens, fewer invasive Aspergillus and Candida infections have been observed. [97] This is in contrast to cryptococcal disease, the incidence of which appears to have been unchanged in SOT recipients.
Major trends that have been observed for cryptococcal disease in SOT recipients include an increased number of older patients and a greater use of tacrolimus-based regimens; also, limited pulmonary disease was noted with greater frequency than meningitis or disseminated disease patterns than were seen previously (possibly owing to the decreased use of OKT3 antibody in treating organ rejection and increased use of immunosuppressive regimens that contain calcineurin inhibitors). [98] Importantly, in SOT recipients, cryptococcal antigen assays may yield false-positive findings because of cross-reaction of Trichosporon beigelii. [99]
Finally, P jiroveci infection [100] often progresses to life-threatening pneumonitis in SOT recipients, especially those with impaired cellular immunity, as in persons with HIV infection/AIDS. SOT recipients undergoing lung or heart-lung transplants are especially at risk, often presenting with fever and nonspecific pulmonary symptoms within 2-6 months posttransplantation. The overall pathogen burden may be lower in SOT recipients than in individuals with HIV infection/AIDS, and the presentations may be more subtle, potentially contributing to delayed or erroneous diagnosis. Despite clinical experience suggesting pathognomonic radiographic patterns associated with P jiroveci pneumonia, no such evidence exists.
Most significant organisms (common and uncommon) observed in solid organ transplant recipients
The list below provides a functionally useful listing of the most significant organisms observed in SOT recipients. The information is largely tabulated from the American Society of Microbiology (ASM) monograph "Infections in Solid-Organ Transplant Recipients," [101] as well as other sources (eg, case reports) for completeness. Although the list is not all-inclusive, it does attempt to capture the common and uncommon pathogens that are of clinical significance to practicing clinicians who manage infections in SOT recipients.
Organisms are listed mostly alphabetically and within functionally useful groupings; no prioritization by prevalence or incidence is implied. All hyperlinks refer to available Medscape Reference articles.
Bacteria
Gram-negative organisms include Acinetobacter species [102] , Burkholderia species, Enterobacteriaceae (E coli, Klebsiella, [28] Enterobacter species), Pseudomonas species, Proteus species, Salmonella and other potentially foodborne pathogens (eg, Campylobacter, Plesiomonas, Shigella species, Vibrio species, Yersinia species), H pylori, and Bacteroides species.
Gram-positive organisms include S aureus (including MRSA), Staphylococcus epidermidis, enterococci, S pneumoniae, group B Streptococcus, Streptococcus milleri, Streptococcus suis, Rhodococcus equi, Corynebacterium urealyticum [103] , Lactobacillus species, Rothia species (eg, Rothia dentocariosa), C difficile, M tuberculosis,Mycobacterium bovis, and atypical mycobacteria. [104]
Other respiratory pathogens include H influenzae, Moraxella catarrhalis, Mycoplasma species, Legionella, and Bordetella.
Other bacteria include Listeria species, Nocardia species, Borrelia species, Neisseria meningitidis, Treponema pallidum species (syphilis), Rickettsia species, Anaplasma phagocytophilum, Bartonella, Coxiella burnetii, Ehrlichia species, Francisella tularensis, and Leptospira species.
Viruses
Herpesviridae include CMV, EBV, HHV-6, HHV-7, HHV-8, and varicella-zoster virus.
Zoonotic viruses include Nipah virus, rabies, arenavirus, LCMV, West Nile virus and other arboviruses, and parapox virus.
Gastrointestinal/viral hepatitis viruses include hepatitis C virus, hepatitis A virus, hepatitis B virus, hepatitis E virus, rotavirus [105] , and noroviruses. [106]
Respiratory viruses [107, 108] include adenovirus, bocavirus, coronaviruses (severe acute respiratory syndrome),influenza [109] , H5N1, metapneumovirus, respiratory syncytial virus, parainfluenza, enteroviruses, HIV, HTLV 1 and 2, and parvovirus B19.
Other viruses (vaccine-preventable) include measles, mumps, rubella, polio, and Japanese encephalitis virus.
Fungi
Opportunistic systemic fungi include Candida species and Cryptococcus. [110]
Geographically endemic species include coccidioidomycosis, histoplasmosis, blastomycosis, and paracoccidioidomycosis.
Invasive molds include Aspergillus species, Fusarium species, Scedosporium, zygomycosis, Mucor species, entomophthoramycosis (eg, Basidiobolus), P jiroveci (previously P carinii), penicilliosis (P marneffei), phaeohyphomycetes (dematiaceous fungi), Sporothrix schenckii, Malassezia species, and Trichosporon.
Parasites
Protozoa include Toxoplasma species, trypanosomiasis (T cruzi [Chagas disease], T brucei [sleeping sickness] [primarily in heart and lung recipients]), Acanthamoeba, Cryptosporidium infection, [111] Giardia species, Microsporidia species, and Isospora. [112]
Tissue and blood protozoa include leishmaniasis (visceral), Plasmodia species (malaria), and Babesia species.
Helminths include Strongyloides stercoralis, Clonorchis sinensis, Echinococcus species, T solium, amebiasis, and Schistosoma species.
Approach to the Febrile Solid Organ Transplant Recipient
The febrile solid organ transplantation (SOT) recipient presents one of the most challenging diagnostic and management situations facing clinicians. [18] Diagnoses must be made accurately, evaluations must be rapidly performed, and management (often empiric) must be effective. The complexity of host immune and metabolic factors, pharmacokinetic issues (eg, drug interactions), [113] a broad range of opportunistic pathogens and processes, difficulties in clinical presentations, and uncertainties in evaluation and therapeutic decision-making are major factors. Nevertheless, a logical framework that provides guidance to clinicians is possible.
A strategic approach to fever (and associated organ system–related manifestations) in the SOT recipient includes the following:
-
Careful evaluation of organ-specific considerations
-
Recognition of specific associations (This can be particularly useful in SOT recipients who present with nonspecific febrile illnesses.)
-
Conducting a thorough clinical assessment using the CREDIT mnemonic (outlined in Framework for Infection Risk Assessment), with special attention to historical clues and physical examination
-
Following a tailored initial diagnostic evaluation
The first consideration in the evaluation of a febrile SOT recipient (or even an afebrile patient in whom infection is suspected) is to review the timeframe around specific infections occurring after transplantation, as presented in the image above. It is advisable to think syndromically (eg, nonspecific febrile illness, pneumonia, urinary tract, [114] CNS [110] ) at first and then narrow the differential diagnoses of possible organisms that could cause the clinical presentation(s). It is important to keep in mind that the clock can get reset based on interim rejection episodes or major immunosuppression due to regimen changes.
Secondly, clinicians should remain aware of the specific types of infection that are associated with specific types of transplantations. For example, kidney transplant recipients are at high risk for genitourinary infections, including pyelonephritis (due to surgical anatomic changes, reflux). [115] BK virus infection is a particular concern. [116]
Surgical wound infections, bloodstream infections, and pneumonia can all result from the usual healthcare-associated pathogens in the first month after transplantation. Subsequently, other syndromes involving opportunistic pathogens, including CMV, may occur, as well as a range of bacteria, viruses, fungi, and parasites, especially in the first 6 months after SOT (see Most significant organisms [common and uncommon] observed in solid organ transplant recipients).
Liver transplant recipients may also be at risk for anastomotic leaks, wound infections, intra-abdominal abscesses, and bacteremia from a host of enteric organisms in addition to the risks of healthcare-associated infections in the postoperative period. [117]
One study reviewed the clinical and microbiology records of 737 patients who received liver transplantation from January 1997 to March 2006. After a median follow-up of 5.8 years, 16.7% developed bacteremia, with 12.5% having gram-positive bacteremia (GPB) and 6.4% having gram-negative bacteremia (GNB). Nosocomial bacteremia, peritonitis, and wound infections were more common in early-onset GPB or GNB patients than patients with late-onset GPB or GNB. The most common pathogens in patients with early-onset GPB were Staphylococcus aureus and Enterococcus faecium.The most common pathogens in late-onset GPB were Enterococcus faecalis and streptococcal species. In early-onset GNB, the most common were anaerobes and P aeruginosa, with E coli being the most common in late-onset GNB. [118]
Heart transplant recipients may more easily develop pneumonia syndromes with associated bacteremia and septic presentations, caused by not only bacteria (eg, Legionella) but also fungi (Aspergillus and Pneumocystis). Sternal wound infections and mediastinitis may occur with increased frequency given the obvious thoracic location of surgical intervention. Additionally, toxoplasmosis often complicates cardiac transplantation because of the latent reservoirs of Toxoplasma cysts in heart muscle; secondary Toxoplasma encephalitis can also occur.
Lung transplantation is most commonly complicated by pneumonia due to presurgical colonization, aspiration, and ventilator support. Local compromises in mucociliary escalator–related clearance mechanisms and airway inflammation likely contribute to the development of infections with both common and uncommon respiratory pathogens in lung transplant recipients. Aspergillus and other molds are usually implicated in single-lung transplantation; prophylactic regimens in these patients likely play an important role.
Thirdly, in SOT recipients who present with an occult fever pattern unaccompanied by specific organ-based symptoms (eg, cough, abdominal pain), clinicians should consider several organisms listed in Most significant organisms (common and uncommon) observed in solid organ transplant recipients that could cause such presentations, including bacterial infections such as Bartonella -associated bacillary angiomatosis; endocarditis; tuberculosis, deep-seated Nocardia infection; herpes simplex virus, EBV, CMV, and HHV-6 infections; fungal complications such as Aspergillus syndromes; or even parasitic infections including visceral leishmaniasis. Noninfectious conditions such as rejection, PTLD, or drug fever should also be considered. Studies have shown that focal origins for febrile illnesses are not evident in up to 25% of cases, lending further support to the search for ancillary clues.
Fourthly, using the CREDIT framework described in Framework for Infection Risk Assessment, the clinician should carefully solicit the important clues underlying key historical features, including any local community-acquired pathogens with or without a seasonal predilection, possibilities for reactivation of specific pathogens (in donor or recipient), important epidemiologically relevant exposures, important donor-derived infections, unfortunate iatrogenic (healthcare-associated) complications, and pertinent travel (on a recent or remote basis).
Based on even a preliminary assessment of timing and nature of illness onset and presentation relative to the transplantation procedure, it is critical to keep an initial syndromic differential diagnoses so all the right questions can be asked, given the major significance of history-taking in the field of infectious disease. [35] Additionally, the physical examination is an important tool that should be thorough and timely, and it may be necessary to repeat the examination often, hour by hour or day to day, depending on the pace and severity of illness. This is even more important given the finding that diagnostic errors are associated with length of stays in, for example, the intensive care unit, a setting in which too little attention is often paid to the physical examination. [119]
Ideally, information from the examination should be derived directly rather than from other team members. Data suggest that two thirds of missed diagnoses in the ICU in one study were infectious in origin. [119] A particularly ominous finding was that disagreement in antemortem and postmortem diagnoses was greater in transplant recipients than in trauma or cardiac surgical patients.
A methodical approach includes starting with assessment of the vital signs, including observing any pulse-temperature dissociation (indicative of noninfectious processes, endocrine illness, or intracellular pathogens). A complete assessment of mucosal surfaces, including the oral cavity, should be performed. Many oral lesions, including dental and gum health, provide insight into likely etiologies and nutritional status. Inflammatory signs may be blunted given the net state of immunosuppression, as in the case of the neutropenic host. A search for invasive devices and evidence of recent procedures is advisable. The presence or absence of a cardiac murmur and peripheral stigmata of endovascular infection need to be determined. The abdominal examination is considered critical, especially in patients who underwent liver transplantation; evidence of surgical leaks, intraabdominal processes, and peritonitis can be lifesaving.
Consider performing pupillary dilation as part of a complete retinal examination, as it may offer clues to a disseminated disease process or increased intracranial pressure associated with a CNS syndrome. As in other immunocompromised hosts, the skin examination is paramount, since many infections leave a dermal footprint through many different types of lesions, including macules, papules, erythema patterns, fluctuance, petechiae, and eschars that correspond to primary infections or secondary complications from dissemination. An extremely helpful medical diagnostic decision program is available online and for handheld devices (including smart phones) for point-of-access differential diagnostic help in the evaluation of any skin lesion. [120]
Finally, as per a recent article on SOT-related infections, Fischer (2006) put forth a tabular summary of recommended initial diagnostic evaluations. [121] It is reproduced here (with permission and slight modification) for its practical value and comprehensive approach.
Modified approach to diagnosis of infection in solid organ transplant recipients with fever
This section describes the recommended initial diagnostic evaluation in patients with various syndromes. [121]
The recommended initial diagnostic evaluation for fever without localizing findings is as follows:
-
Urinalysis and urine culture
-
Chest radiography
-
Blood cultures
-
CMV PCR
-
Purified protein derivative (PPD) (Consider QuantiFERON testing using interferon gamma assays.)
-
Antigen detection tests available for adenovirus, influenza A, respiratory syncytial virus, and rotavirus; PCR may also be available
The recommended initial diagnostic evaluation for pulmonary infiltrates (alveolar pattern) is as follows:
-
PPD (consider QuantiFERON testing using interferon gamma assays)
-
Blood cultures
-
Sputum Gram stain and culture
-
Urine Legionella and pneumococcal antigens
-
Sputum acid-fast bacillus (AFB) smear and culture (DNA probes if available)
-
Urine Histoplasma antigen [99] in endemic areas or suggestive travel
-
Bronchoscopy if fever and infiltrates persist
The recommended initial diagnostic evaluation for pulmonary infiltrates (interstitial pattern) is as follows:
-
Workup for pulmonary infiltrates (alveolar pattern) plus CMV PCR
-
Coccidioides serology, if warranted
-
Bronchoscopy with transbronchial biopsy if fever and infiltrates persist
The recommended initial diagnostic evaluation for CNS symptoms is as follows:
-
Brain MRI (with gadolinium)
-
Lumbar puncture for CSF analysis: usual studies (cell count and differential); glucose, protein; bacterial, viral, fungal, [99, 122] AFB cultures, cryptococcal antigen, and several PCR probes (eg, herpes simplex virus) that may be available and relevant; and cytology
-
Consider PCR and serology for other pathogens (CMV, EBV, WNV), arboviral testing
-
Biopsy of mass lesions and/or leptomeninges (especially to identify granulomatous meningitis)
The recommended initial diagnostic evaluation for diarrhea is as follows:
-
Stool for WBC and cultures (for enteric [Salmonella, Shigella, Campylobacter)
-
At least 2 separate stool specimens for C difficile testing (enzyme immunoassay [EIA] acceptable)
-
Three separate stool specimens for ova and parasites
-
CMV PCR (blood)
-
If stool studies unrevealing and diarrhea persists, endoscopic evaluation warranted (with mucosal biopsy); immunohistochemical staining for CMV should be performed
The recommended initial diagnostic evaluation for lymphadenopathy is as follows:
-
EBV PCR, CMV PCR (blood)
-
Bartonella (catscratch disease) serology
-
T gondii serology
-
PPD (consider QuantiFERON testing using interferon gamma assays)
-
Biopsy of involved lymph node is often diagnostic and performed quickly to exclude PTLD and occult infections (eg, tuberculosis); node tissue should be submitted for histologic examination to look for atypical cells, granulomata, and cultures (aerobic, anaerobic, AFB, fungal and modified AFB)
-
CT scanning of neck, chest, abdomen, and pelvis might be useful to demonstrate the extent of nodal involvement.
Special Host Considerations
Two types of hosts are discussed here for their significance in the solid organ transplantation (SOT) context: the pediatric patient [123, 124, 125] and the HIV-positive patient. [126]
Pediatric patients
The younger the child (especially infants), the greater the risk of infections, and, often, the more severe the disease. [123] Age is a determinant, especially because younger age groups are often at risk for certain types of natural infection, and primary immunization series may not have been completed by the time of transplantation. In one of the largest pediatric SOT cohorts, some risk factors for bacterial and fungal infections included age (highest risk among infants), race (black and Hispanic), use of cyclosporine as a first immunosuppressive agent, and increasing bilirubin levels, among others. [123] Most common etiologies were viruses, including CMV, EBV, HHV-6, HHV-7, [124] parvovirus B19, [125] adenovirus, human metapneumovirus, and polyomavirus.
Viral infections are often associated with rejection, allograft dysfunction, vasculopathy, and poor prognosis. Primary varicella-zoster virus infection can often disseminate to visceral organs. In a cardiac transplant study, respiratory infections were most frequently encountered, followed by infections in the urinary tract, gastrointestinal tract, and then CNS. Bacterial infections are often associated with invasive devices; rarely, unusual organisms such as R dentocariosa are seen. [127] Nontuberculous mycobacteria have been isolated in up to 8% of BAL specimens in some studies.
Based on usual recommendations from agencies such as the CDC, most vaccines should ideally be given before transplantation. Vaccine titers can rapidly decline after SOT, and more research is needed on ways to maintain immune response. [128] Since pediatric rashes are common even in the general population, such infections may have similar presentations in pediatric SOT recipients. However, other skin lesions may be atypical and could represent dissemination, drug hypersensitivity, or organ rejection.
HIV-infected patients
In an important review, Roland and Stock discuss SOT issues as they relate to the HIV-positive patient. [129] Given the overwhelming success of highly active antiretroviral therapy in improving longevity and quality of life for individuals infected with HIV, the primary questions related to SOT in this population concern optimal candidacy and methods of effective management following SOT. [130]
Despite overall comparable graft survival rates, allograft rejection is noted to occur with kidney transplants in HIV-positive patients. [129] To compound the challenges, antirejection therapies have been subsequently associated with severe non–AIDS-defining conditions. Some recommendations to prevent post-SOT infections have empiric rationale, including the advisability of using secondary prophylaxis immediately after SOT, regardless of T-cell counts. [129] Screening for opportunistic infections should be vigorous, including monitoring for both HIV-associated infections and other types of infections seen in SOT recipients.
Infection Prevention Strategies
The key infection-prevention strategies in solid organ transplantation (SOT) recipients include (1) improving adherence to the eligibility criteria for deceased donor organ donation, [131, 132] (2) primary or preemptive prophylaxis with antimicrobials and vaccination, [133, 35, 134, 68, 135, 136] and (3) promoting healthy behaviors and risk reduction in various settings post-SOT (eg, adherence to pretravel consultation for SOT recipients, infection-control recommendations in healthcare or home settings).Although there are 2 excellent recent reviews on general recommendations for prudent infection prevention and immunization practices in SOT recipients, [137, 138] many resources are available to guide patients and providers in these areas, including the following:
-
Kotton CN, Ryan ET, Fishman JA. Prevention of infection in adult travelers after solid organ transplantation. Am J Transplant. Jan 2005;5(1):8-14. [QxMD MEDLINE Link]
-
Kotton CN, Hibberd PL. Travel medicine and the solid organ transplant recipient. Am J Transplant. Dec 2009;9 Suppl 4:S273-81. [QxMD MEDLINE Link]
-
Trubiano JA, Johnson D, Sohail A, Torresi J. Travel vaccination recommendations and endemic infection risks in solid organ transplantation recipients. J Travel Med. 2016 Jun. 23 (6). [QxMD MEDLINE Link]
Infection-control practices must be optimized for SOT recipients and providers. The CDC provides several guidelines for effective infection control measures here. Although many of the policies and procedures relate to specific setting and types of exposure, the most important and cost-effective tool available to all individuals, especially SOT recipients and their families and loved ones, is hand hygiene. A great deal of information on proper technique is available from the CDC here, in addition to guidance for the range of questions that concern hand hygiene methods, materials, and best practices.
-
Schematic sites of action of common immunosuppressants. Image courtesy of Elsevier.
-
Changing timeline of infection after organ transplantation (modified from Fishman J. NEJM. 2007;357(25):2601-14).
Tables
What would you like to print?
- Practice Essentials
- Background Concepts
- Immunosuppressive Drugs Used in Solid Organ Transplantation
- Statins
- Timeframe
- Framework for Infection Risk Assessment
- Selected Pathogens of Clinical Significance in Solid Organ Transplant Recipients
- Approach to the Febrile Solid Organ Transplant Recipient
- Special Host Considerations
- Infection Prevention Strategies
- Show All
- Media Gallery
- References