-
PDF
- Split View
-
Views
-
Cite
Cite
Susanna C. Larsson, Nicola Orsini, Red Meat and Processed Meat Consumption and All-Cause Mortality: A Meta-Analysis, American Journal of Epidemiology, Volume 179, Issue 3, 1 February 2014, Pages 282–289, https://doi.org/10.1093/aje/kwt261
Close - Share Icon Share
Abstract
High consumption of red meat and processed meat has been associated with increased risk of several chronic diseases. We conducted a meta-analysis to summarize the evidence from prospective studies on red meat and processed meat consumption in relationship to all-cause mortality. Pertinent studies were identified by searching PubMed through May 2013 and by reviewing the reference lists of retrieved articles. Prospective studies that reported relative risks with 95% confidence intervals for the association of red meat or processed meat consumption with all-cause mortality were eligible. Study-specific results were combined by using a random-effects model. Nine prospective studies were included in the meta-analysis. The summary relative risks of all-cause mortality for the highest versus the lowest category of consumption were 1.10 (95% confidence interval (CI): 0.98, 1.22; n = 6 studies) for unprocessed red meat, 1.23 (95% CI: 1.17, 1.28; n = 6 studies) for processed meat, and 1.29 (95% CI: 1.24, 1.35; n = 5 studies) for total red meat. In a dose-response meta-analysis, consumption of processed meat and total red meat, but not unprocessed red meat, was statistically significantly positively associated with all-cause mortality in a nonlinear fashion. These results indicate that high consumption of red meat, especially processed meat, may increase all-cause mortality.
Accumulating evidence indicates that high consumption of red meat and processed meat may increase the risk of chronic diseases, such as type 2 diabetes (1), cardiovascular disease (1–4), and certain cancers (2, 4–7). Recent large prospective studies have found that red meat and processed meat consumption is associated with increased risk of all-cause mortality (2, 4, 8). Because the evidence from prospective studies on red meat and processed meat consumption in relationship to all-cause mortality has not yet been summarized, we conducted a systematic review with meta-analysis to quantify the association.
MATERIALS AND METHODS
Literature search
We followed standard criteria for conducting and reporting of meta-analyses of observational studies (9). Studies were identified through a systematic review of the literature (through May 2013) by using the electronic PubMed database (http://www.ncbi.nlm.nih.gov/pubmed) without restrictions. We used the search terms “meat,” “beef,” “pork,” “veal,” “lamb,” “steak,” “hamburger,” “ham,” “bacon,” or “sausage” in combination with “mortality” or “death.” In addition, we searched the reference lists of relevant publications for more studies.
Study selection
We included prospective studies that reported relative risks with their 95% confidence intervals for the associations of unprocessed red meat, processed meat, and/or total red meat consumption with all-cause mortality. “Unprocessed red meat” was defined as unprocessed beef, pork, lamb, or game, excluding fish and poultry. “Processed meat” was defined as any meat preserved by smoking, salting, curing, or by the addition of chemical preservatives, such as bacon, sausages, hot dogs, salami, or ham. “Total red meat” was defined as unprocessed red meat and processed meat combined. Studies comparing the mortality rates in vegetarians with those of nonvegetarians were not included. We also omitted studies that examined only cause-specific mortality such as cardiovascular or cancer mortality, as well as studies that reported results for total meat (red and white meat combined) consumption only.
Data extraction
From each publication, we extracted the first author's last name, year of publication, study location, sex, age, sample size (number of deaths and total number of participants), years of follow-up, relative risks with 95% confidence intervals for each category of red meat intake, and covariates adjusted for in the analysis. We extracted the relative risk estimates from the most fully adjusted multivariable model. Data were extracted separately for men and women if possible. Two researchers (S.C.L. and N.O.) independently reviewed articles and extracted information.
Data synthesis and analysis
In addition to combining the risk estimates for the highest versus lowest consumption category, we also estimated for each study the relative risk and 95% confidence interval for an increment of 100 g/day of unprocessed red meat and total red meat consumption and for an increment of 50 g/day of processed meat consumption and combined those estimates. For the dose-response meta-analysis, the method proposed by Greenland and Longnecker (10) and Orsini et al. (11) was used to compute the trend from the correlated log relative risks across categories of meat consumption. This method requires that 1) the number of deaths and total number of participants (or person-time) for each category are known; 2) the relative risks with confidence intervals are presented for at least 2 exposure categories; and 3) the mean or median meat consumption for each category is either reported in the article or can be estimated. We assigned the mean or median meat consumption for each category to the corresponding relative risk. When meat consumption was reported in servings (4) or frequency (12), we estimated the consumption in grams by using the standard serving size for unprocessed red meat (85 g) reported by Pan et al. (4) and assumed that 1 serving of processed meat and total red meat corresponded to 30 g and 85 g, respectively. Risk estimates from individual studies were combined with the method of DerSimonian and Laird by using the assumptions of a random-effects model (13), which considers both within-study and between-study variation (weighting was based on the inverse of the variance).
Nonlinear associations between meat consumption and all-cause mortality were tested by using a 2-stage random-effects dose-response meta-analysis (11, 14). Meat consumption was modeled by using restricted cubic splines with 3 knots (2 spline transformations) at fixed percentiles (10%, 50%, and 90%) of the distribution. A P value for nonlinearity was obtained by testing the regression coefficient of the second spline equal to 0 (15).
Heterogeneity among studies was evaluated by using the Q and I2 statistics (16). We performed analyses stratified by sex and geographical area (United States and Europe). Small study bias, such as publication bias, was explored by visual inspection of funnel plots and formal testing by using Egger's test (17). All statistical analyses were conducted by using Stata, version 12, software (StataCorp LP, College Station, Texas). P values of less than 0.05 were considered statistically significant.
RESULTS
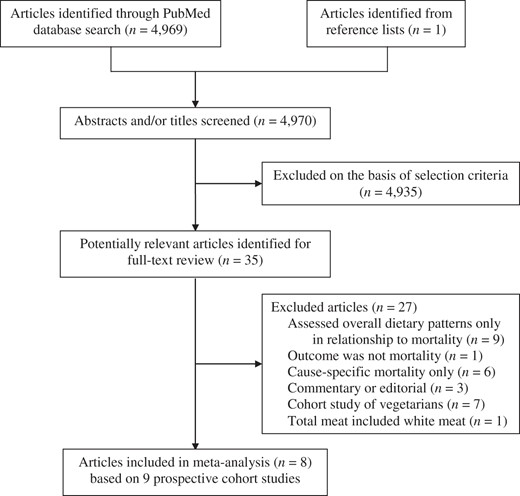
Nine prospective studies (2, 4, 8, 12, 18–21) (1 article presented results from 2 independent cohorts (4)) of unprocessed red meat (n = 6 studies), processed meat (n = 6 studies), and/or total red meat (n = 5 studies) consumption in relationship to all-cause mortality fulfilled our inclusion criteria (Figure 1). Characteristics of the 9 studies are presented in Table 1. Combined, these studies included 1,330,352 individuals and 137,376 deaths. Five studies were conducted in the United States, 3 in Europe, and 1 in China. All studies adjusted for age, sex (if applicable), and smoking. Most studies also controlled for physical activity (n = 8 studies), alcohol consumption (n = 8 studies), total energy intake (n = 7 studies), body mass index (weight (kg)/height (m)2) or body weight (n = 7 studies), and markers of socioeconomic status (n = 5 studies).
Characteristics of Prospective Studies of Unprocessed Red Meat, Processed Meat, and Total Red Meat Consumption and All-Cause Mortality
| First Author, Year (Reference No.) . | Cohort Name . | Location of Study . | No. of Deaths . | Cohort Sizea . | Sex . | Age, Years . | Follow-up, Years . | Dietary Assessment Method . | Year(s) of Assessment . | Type of Meat . | Adjustments . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Highest Intake Category . | Lowest Intake Category . | |||||||||||
| Whiteman, 1999 (12) | OXCHECK Study | United Kingdom | 598 | 10,522 | Men and women | 35−64 | 9 | 11-Item FFQ | 1989 | Unprocessed red meat: 4−7 days/week | Unprocessed red meat: <1 day/week | Age; sex; smoking |
| Processed meat: 4−7 days/week | Processed meat: <1 day/week | |||||||||||
| Kelemen, 2005 (18) | IWHS | United States | 3,978 | 29,017 | Women | 55−69 | 15 | 127-Item SQ-FFQ | 1986 | Total red meat: 1.20 servings/1,000 kcal | Total red meat: 0.28 servings/1,000 kcal | Age; education; smoking; physical activity; BMIb; hypertension; postmenopausal hormone use; multivitamin and vitamin E supplement use; family history of cancer; intakes of total energy, alcohol, saturated fat, monounsaturated fat, polyunsaturated fat, trans-fat, dietary cholesterol, methionine, total fiber, fruits and vegetables, legumes, dairy, eggs, poultry, and fish |
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 47,976 | 322,263 | Men | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcal2 | Processed meat: 2.2 g/1,000 kcal2 | Age; race; education; marital status; smoking; physical activity; BMI; vitamin supplement use; intakes of total energy, alcohol, fruits, and vegetables |
| Total meat: 68.1 g/ 1,000 kcal | Total meat: 9.3 g/ 1,000 kcal | |||||||||||
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 23,276 | 223,390 | Women | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcalc | Processed meat: 2.2 g/1,000 kcalc | As above and additionally for hormone replacement therapy |
| Total meat: 65.9 g/ 1,000 kcal | Total meat: 9.1 g/ 1,000 kcal | |||||||||||
| Trichopoulou, 2009 (19) | NA | Greece | 652 | 23,349 | Men and women | 20−86 | 8.5 | 150-Item SQ-FFQ | 1994−1997 | Total meat: ≥mediand | Total meat: <mediand | Age; sex; education; smoking; physical activity; BMI; waist-to-hip ratio; intakes of total energy, alcohol, ratio of monounsaturated to saturated lipids, fruits and nuts, vegetables, legumes, cereals, fish and seafood, and dairy products |
| Pan, 2012 (4) | HPFS | United States | 8,926 | 37,698 | Men | 40−75 | 22 | 131- to 166-Item SQ-FFQs | 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.46 servings/day | Unprocessed red meat: 0.17 servings/day | Age; race; smoking; physical activity; BMI; family history of diabetes, myocardial infarction or cancer; history of diabetes, hypertension or hypercholesterolemia; intakes of total energy, alcohol, whole grains, fruits, and vegetables |
| Processed meat: 0.74 servings/day | Processed meat: 0.02 servings/day | |||||||||||
| Total red meat: 2.07 servings/day | Total red meat: 0.25 servings/day | |||||||||||
| Pan, 2012 (4) | NHS | United States | 15,000 | 83,644 | Women | 30−55 | 28 | 61- to 166-Item SQ-FFQs | 1984, 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.64 servings/day | Unprocessed red meat: 0.37 servings/day | As above and additionally for menopausal status and postmenopausal hormone use |
| Processed meat: 0.64 servings/day | Processed meat: 0.05 servings/day | |||||||||||
| Total red meat: 2.17 servings/day | Total red meat: 0.51 servings/day | |||||||||||
| Takata, 2013 (20) | SMHS | China | 2,733 | 61,128 | Men | 40−74 | 5.5 | 81-Item FFQ | 2002−2006 | Unprocessed red meat: 126.0 g/day | Unprocessed red meat: 21.4 g/day | Age; income; education; occupation; comorbidity index; smoking; physical activity; intakes of total energy, alcohol, fruits, vegetables, fish, poultry, and pork |
| Takata, 2013 (20) | SWHS | China | 4,210 | 73,162 | Women | 40−70 | 11.2 | 77-Item FFQ | 1997−2000 | Unprocessed red meat: 103.4 g/day | Unprocessed red meat: 16.5 g/day | As above but not alcohol |
| Rohrmann, 2013 (8) | EPIC | 10 European countries | 26,344 | 448,568 | Men and women | 35−69 | 12.7 | FFQ in most studies | NA | Unprocessed red meat: ≥160 g/day | Unprocessed red meat: 15 g/day | Age; sex; study center; education; smoking; physical activity; body weight; height; intakes of total energy, alcohol, and poultry |
| Processed meat: ≥160 g/day | Processed meat: 15 g/day | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,908 | 8,239 | Men | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | Age; race; socioeconomic status; marital status; smoking; physical activity; BMI; history of diabetes, hypertension, or hypercholesterolemia; family history of diabetes or hypercholesterolemia; use of aspirin or ibuprofen; use of mineral and vitamin supplements; intakes of alcohol and fruit and vegetables |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,775 | 9,372 | Women | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | As above and additionally for use of oral contraceptives and hormone replacement therapy |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| First Author, Year (Reference No.) . | Cohort Name . | Location of Study . | No. of Deaths . | Cohort Sizea . | Sex . | Age, Years . | Follow-up, Years . | Dietary Assessment Method . | Year(s) of Assessment . | Type of Meat . | Adjustments . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Highest Intake Category . | Lowest Intake Category . | |||||||||||
| Whiteman, 1999 (12) | OXCHECK Study | United Kingdom | 598 | 10,522 | Men and women | 35−64 | 9 | 11-Item FFQ | 1989 | Unprocessed red meat: 4−7 days/week | Unprocessed red meat: <1 day/week | Age; sex; smoking |
| Processed meat: 4−7 days/week | Processed meat: <1 day/week | |||||||||||
| Kelemen, 2005 (18) | IWHS | United States | 3,978 | 29,017 | Women | 55−69 | 15 | 127-Item SQ-FFQ | 1986 | Total red meat: 1.20 servings/1,000 kcal | Total red meat: 0.28 servings/1,000 kcal | Age; education; smoking; physical activity; BMIb; hypertension; postmenopausal hormone use; multivitamin and vitamin E supplement use; family history of cancer; intakes of total energy, alcohol, saturated fat, monounsaturated fat, polyunsaturated fat, trans-fat, dietary cholesterol, methionine, total fiber, fruits and vegetables, legumes, dairy, eggs, poultry, and fish |
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 47,976 | 322,263 | Men | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcal2 | Processed meat: 2.2 g/1,000 kcal2 | Age; race; education; marital status; smoking; physical activity; BMI; vitamin supplement use; intakes of total energy, alcohol, fruits, and vegetables |
| Total meat: 68.1 g/ 1,000 kcal | Total meat: 9.3 g/ 1,000 kcal | |||||||||||
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 23,276 | 223,390 | Women | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcalc | Processed meat: 2.2 g/1,000 kcalc | As above and additionally for hormone replacement therapy |
| Total meat: 65.9 g/ 1,000 kcal | Total meat: 9.1 g/ 1,000 kcal | |||||||||||
| Trichopoulou, 2009 (19) | NA | Greece | 652 | 23,349 | Men and women | 20−86 | 8.5 | 150-Item SQ-FFQ | 1994−1997 | Total meat: ≥mediand | Total meat: <mediand | Age; sex; education; smoking; physical activity; BMI; waist-to-hip ratio; intakes of total energy, alcohol, ratio of monounsaturated to saturated lipids, fruits and nuts, vegetables, legumes, cereals, fish and seafood, and dairy products |
| Pan, 2012 (4) | HPFS | United States | 8,926 | 37,698 | Men | 40−75 | 22 | 131- to 166-Item SQ-FFQs | 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.46 servings/day | Unprocessed red meat: 0.17 servings/day | Age; race; smoking; physical activity; BMI; family history of diabetes, myocardial infarction or cancer; history of diabetes, hypertension or hypercholesterolemia; intakes of total energy, alcohol, whole grains, fruits, and vegetables |
| Processed meat: 0.74 servings/day | Processed meat: 0.02 servings/day | |||||||||||
| Total red meat: 2.07 servings/day | Total red meat: 0.25 servings/day | |||||||||||
| Pan, 2012 (4) | NHS | United States | 15,000 | 83,644 | Women | 30−55 | 28 | 61- to 166-Item SQ-FFQs | 1984, 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.64 servings/day | Unprocessed red meat: 0.37 servings/day | As above and additionally for menopausal status and postmenopausal hormone use |
| Processed meat: 0.64 servings/day | Processed meat: 0.05 servings/day | |||||||||||
| Total red meat: 2.17 servings/day | Total red meat: 0.51 servings/day | |||||||||||
| Takata, 2013 (20) | SMHS | China | 2,733 | 61,128 | Men | 40−74 | 5.5 | 81-Item FFQ | 2002−2006 | Unprocessed red meat: 126.0 g/day | Unprocessed red meat: 21.4 g/day | Age; income; education; occupation; comorbidity index; smoking; physical activity; intakes of total energy, alcohol, fruits, vegetables, fish, poultry, and pork |
| Takata, 2013 (20) | SWHS | China | 4,210 | 73,162 | Women | 40−70 | 11.2 | 77-Item FFQ | 1997−2000 | Unprocessed red meat: 103.4 g/day | Unprocessed red meat: 16.5 g/day | As above but not alcohol |
| Rohrmann, 2013 (8) | EPIC | 10 European countries | 26,344 | 448,568 | Men and women | 35−69 | 12.7 | FFQ in most studies | NA | Unprocessed red meat: ≥160 g/day | Unprocessed red meat: 15 g/day | Age; sex; study center; education; smoking; physical activity; body weight; height; intakes of total energy, alcohol, and poultry |
| Processed meat: ≥160 g/day | Processed meat: 15 g/day | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,908 | 8,239 | Men | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | Age; race; socioeconomic status; marital status; smoking; physical activity; BMI; history of diabetes, hypertension, or hypercholesterolemia; family history of diabetes or hypercholesterolemia; use of aspirin or ibuprofen; use of mineral and vitamin supplements; intakes of alcohol and fruit and vegetables |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,775 | 9,372 | Women | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | As above and additionally for use of oral contraceptives and hormone replacement therapy |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
Abbreviations: BMI, body mass index; EPIC, European Prospective Investigation into Cancer and Nutrition; FFQ, food frequency questionnaire; HPFS, Health Professionals Follow-up Study; IWHS, Iowa Women's Health Study; NA, not available; NHANES, National Health and Nutrition Examination Survey; NHS, Nurses’ Health Study; NIH–AARP, National Institutes of Health–AARP (formerly known as the American Association of Retired Persons); OXCHECK, Oxford and Collaborators Health Check; SMHS, Shanghai Men's Health Study; SQ, semiquantitative; SWHS, Shanghai Women's Health Study.
a The numbers may be smaller in the specific analysis of meat consumption.
b Weight (kg)/height (m)2.
c Obtained from another publication based on data from the same cohort (29).
d Median consumption was 121 g/day for men and 90 g/day for women.
Characteristics of Prospective Studies of Unprocessed Red Meat, Processed Meat, and Total Red Meat Consumption and All-Cause Mortality
| First Author, Year (Reference No.) . | Cohort Name . | Location of Study . | No. of Deaths . | Cohort Sizea . | Sex . | Age, Years . | Follow-up, Years . | Dietary Assessment Method . | Year(s) of Assessment . | Type of Meat . | Adjustments . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Highest Intake Category . | Lowest Intake Category . | |||||||||||
| Whiteman, 1999 (12) | OXCHECK Study | United Kingdom | 598 | 10,522 | Men and women | 35−64 | 9 | 11-Item FFQ | 1989 | Unprocessed red meat: 4−7 days/week | Unprocessed red meat: <1 day/week | Age; sex; smoking |
| Processed meat: 4−7 days/week | Processed meat: <1 day/week | |||||||||||
| Kelemen, 2005 (18) | IWHS | United States | 3,978 | 29,017 | Women | 55−69 | 15 | 127-Item SQ-FFQ | 1986 | Total red meat: 1.20 servings/1,000 kcal | Total red meat: 0.28 servings/1,000 kcal | Age; education; smoking; physical activity; BMIb; hypertension; postmenopausal hormone use; multivitamin and vitamin E supplement use; family history of cancer; intakes of total energy, alcohol, saturated fat, monounsaturated fat, polyunsaturated fat, trans-fat, dietary cholesterol, methionine, total fiber, fruits and vegetables, legumes, dairy, eggs, poultry, and fish |
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 47,976 | 322,263 | Men | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcal2 | Processed meat: 2.2 g/1,000 kcal2 | Age; race; education; marital status; smoking; physical activity; BMI; vitamin supplement use; intakes of total energy, alcohol, fruits, and vegetables |
| Total meat: 68.1 g/ 1,000 kcal | Total meat: 9.3 g/ 1,000 kcal | |||||||||||
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 23,276 | 223,390 | Women | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcalc | Processed meat: 2.2 g/1,000 kcalc | As above and additionally for hormone replacement therapy |
| Total meat: 65.9 g/ 1,000 kcal | Total meat: 9.1 g/ 1,000 kcal | |||||||||||
| Trichopoulou, 2009 (19) | NA | Greece | 652 | 23,349 | Men and women | 20−86 | 8.5 | 150-Item SQ-FFQ | 1994−1997 | Total meat: ≥mediand | Total meat: <mediand | Age; sex; education; smoking; physical activity; BMI; waist-to-hip ratio; intakes of total energy, alcohol, ratio of monounsaturated to saturated lipids, fruits and nuts, vegetables, legumes, cereals, fish and seafood, and dairy products |
| Pan, 2012 (4) | HPFS | United States | 8,926 | 37,698 | Men | 40−75 | 22 | 131- to 166-Item SQ-FFQs | 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.46 servings/day | Unprocessed red meat: 0.17 servings/day | Age; race; smoking; physical activity; BMI; family history of diabetes, myocardial infarction or cancer; history of diabetes, hypertension or hypercholesterolemia; intakes of total energy, alcohol, whole grains, fruits, and vegetables |
| Processed meat: 0.74 servings/day | Processed meat: 0.02 servings/day | |||||||||||
| Total red meat: 2.07 servings/day | Total red meat: 0.25 servings/day | |||||||||||
| Pan, 2012 (4) | NHS | United States | 15,000 | 83,644 | Women | 30−55 | 28 | 61- to 166-Item SQ-FFQs | 1984, 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.64 servings/day | Unprocessed red meat: 0.37 servings/day | As above and additionally for menopausal status and postmenopausal hormone use |
| Processed meat: 0.64 servings/day | Processed meat: 0.05 servings/day | |||||||||||
| Total red meat: 2.17 servings/day | Total red meat: 0.51 servings/day | |||||||||||
| Takata, 2013 (20) | SMHS | China | 2,733 | 61,128 | Men | 40−74 | 5.5 | 81-Item FFQ | 2002−2006 | Unprocessed red meat: 126.0 g/day | Unprocessed red meat: 21.4 g/day | Age; income; education; occupation; comorbidity index; smoking; physical activity; intakes of total energy, alcohol, fruits, vegetables, fish, poultry, and pork |
| Takata, 2013 (20) | SWHS | China | 4,210 | 73,162 | Women | 40−70 | 11.2 | 77-Item FFQ | 1997−2000 | Unprocessed red meat: 103.4 g/day | Unprocessed red meat: 16.5 g/day | As above but not alcohol |
| Rohrmann, 2013 (8) | EPIC | 10 European countries | 26,344 | 448,568 | Men and women | 35−69 | 12.7 | FFQ in most studies | NA | Unprocessed red meat: ≥160 g/day | Unprocessed red meat: 15 g/day | Age; sex; study center; education; smoking; physical activity; body weight; height; intakes of total energy, alcohol, and poultry |
| Processed meat: ≥160 g/day | Processed meat: 15 g/day | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,908 | 8,239 | Men | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | Age; race; socioeconomic status; marital status; smoking; physical activity; BMI; history of diabetes, hypertension, or hypercholesterolemia; family history of diabetes or hypercholesterolemia; use of aspirin or ibuprofen; use of mineral and vitamin supplements; intakes of alcohol and fruit and vegetables |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,775 | 9,372 | Women | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | As above and additionally for use of oral contraceptives and hormone replacement therapy |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| First Author, Year (Reference No.) . | Cohort Name . | Location of Study . | No. of Deaths . | Cohort Sizea . | Sex . | Age, Years . | Follow-up, Years . | Dietary Assessment Method . | Year(s) of Assessment . | Type of Meat . | Adjustments . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Highest Intake Category . | Lowest Intake Category . | |||||||||||
| Whiteman, 1999 (12) | OXCHECK Study | United Kingdom | 598 | 10,522 | Men and women | 35−64 | 9 | 11-Item FFQ | 1989 | Unprocessed red meat: 4−7 days/week | Unprocessed red meat: <1 day/week | Age; sex; smoking |
| Processed meat: 4−7 days/week | Processed meat: <1 day/week | |||||||||||
| Kelemen, 2005 (18) | IWHS | United States | 3,978 | 29,017 | Women | 55−69 | 15 | 127-Item SQ-FFQ | 1986 | Total red meat: 1.20 servings/1,000 kcal | Total red meat: 0.28 servings/1,000 kcal | Age; education; smoking; physical activity; BMIb; hypertension; postmenopausal hormone use; multivitamin and vitamin E supplement use; family history of cancer; intakes of total energy, alcohol, saturated fat, monounsaturated fat, polyunsaturated fat, trans-fat, dietary cholesterol, methionine, total fiber, fruits and vegetables, legumes, dairy, eggs, poultry, and fish |
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 47,976 | 322,263 | Men | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcal2 | Processed meat: 2.2 g/1,000 kcal2 | Age; race; education; marital status; smoking; physical activity; BMI; vitamin supplement use; intakes of total energy, alcohol, fruits, and vegetables |
| Total meat: 68.1 g/ 1,000 kcal | Total meat: 9.3 g/ 1,000 kcal | |||||||||||
| Sinha, 2009 (2) | NIH-AARP Diet and Health Study | United States | 23,276 | 223,390 | Women | 50−71 | 10 | 124-Item FFQ | 1995 | Processed meat: 23.6 g/1,000 kcalc | Processed meat: 2.2 g/1,000 kcalc | As above and additionally for hormone replacement therapy |
| Total meat: 65.9 g/ 1,000 kcal | Total meat: 9.1 g/ 1,000 kcal | |||||||||||
| Trichopoulou, 2009 (19) | NA | Greece | 652 | 23,349 | Men and women | 20−86 | 8.5 | 150-Item SQ-FFQ | 1994−1997 | Total meat: ≥mediand | Total meat: <mediand | Age; sex; education; smoking; physical activity; BMI; waist-to-hip ratio; intakes of total energy, alcohol, ratio of monounsaturated to saturated lipids, fruits and nuts, vegetables, legumes, cereals, fish and seafood, and dairy products |
| Pan, 2012 (4) | HPFS | United States | 8,926 | 37,698 | Men | 40−75 | 22 | 131- to 166-Item SQ-FFQs | 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.46 servings/day | Unprocessed red meat: 0.17 servings/day | Age; race; smoking; physical activity; BMI; family history of diabetes, myocardial infarction or cancer; history of diabetes, hypertension or hypercholesterolemia; intakes of total energy, alcohol, whole grains, fruits, and vegetables |
| Processed meat: 0.74 servings/day | Processed meat: 0.02 servings/day | |||||||||||
| Total red meat: 2.07 servings/day | Total red meat: 0.25 servings/day | |||||||||||
| Pan, 2012 (4) | NHS | United States | 15,000 | 83,644 | Women | 30−55 | 28 | 61- to 166-Item SQ-FFQs | 1984, 1986, 1990, 1994, 1998, 2002, and 2006 | Unprocessed red meat: 1.64 servings/day | Unprocessed red meat: 0.37 servings/day | As above and additionally for menopausal status and postmenopausal hormone use |
| Processed meat: 0.64 servings/day | Processed meat: 0.05 servings/day | |||||||||||
| Total red meat: 2.17 servings/day | Total red meat: 0.51 servings/day | |||||||||||
| Takata, 2013 (20) | SMHS | China | 2,733 | 61,128 | Men | 40−74 | 5.5 | 81-Item FFQ | 2002−2006 | Unprocessed red meat: 126.0 g/day | Unprocessed red meat: 21.4 g/day | Age; income; education; occupation; comorbidity index; smoking; physical activity; intakes of total energy, alcohol, fruits, vegetables, fish, poultry, and pork |
| Takata, 2013 (20) | SWHS | China | 4,210 | 73,162 | Women | 40−70 | 11.2 | 77-Item FFQ | 1997−2000 | Unprocessed red meat: 103.4 g/day | Unprocessed red meat: 16.5 g/day | As above but not alcohol |
| Rohrmann, 2013 (8) | EPIC | 10 European countries | 26,344 | 448,568 | Men and women | 35−69 | 12.7 | FFQ in most studies | NA | Unprocessed red meat: ≥160 g/day | Unprocessed red meat: 15 g/day | Age; sex; study center; education; smoking; physical activity; body weight; height; intakes of total energy, alcohol, and poultry |
| Processed meat: ≥160 g/day | Processed meat: 15 g/day | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,908 | 8,239 | Men | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | Age; race; socioeconomic status; marital status; smoking; physical activity; BMI; history of diabetes, hypertension, or hypercholesterolemia; family history of diabetes or hypercholesterolemia; use of aspirin or ibuprofen; use of mineral and vitamin supplements; intakes of alcohol and fruit and vegetables |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
| Kappeler, 2013 (21) | NHANES III | United States | 1,775 | 9,372 | Women | NA | 22 | 81-Item FFQ | 1988−1994 | Unprocessed red meat: ≥45 times/month | Unprocessed red meat: ≤6 times/month | As above and additionally for use of oral contraceptives and hormone replacement therapy |
| Processed red meat: ≥45 times/month | Processed red meat: ≤6 times/month | |||||||||||
Abbreviations: BMI, body mass index; EPIC, European Prospective Investigation into Cancer and Nutrition; FFQ, food frequency questionnaire; HPFS, Health Professionals Follow-up Study; IWHS, Iowa Women's Health Study; NA, not available; NHANES, National Health and Nutrition Examination Survey; NHS, Nurses’ Health Study; NIH–AARP, National Institutes of Health–AARP (formerly known as the American Association of Retired Persons); OXCHECK, Oxford and Collaborators Health Check; SMHS, Shanghai Men's Health Study; SQ, semiquantitative; SWHS, Shanghai Women's Health Study.
a The numbers may be smaller in the specific analysis of meat consumption.
b Weight (kg)/height (m)2.
c Obtained from another publication based on data from the same cohort (29).
d Median consumption was 121 g/day for men and 90 g/day for women.
Study flow diagram. Studies that were excluded on the basis of selection criteria included experimental studies in animals or in vitro and other nonepidemiologic studies or review articles unrelated to red meat and mortality.
Highest versus lowest category
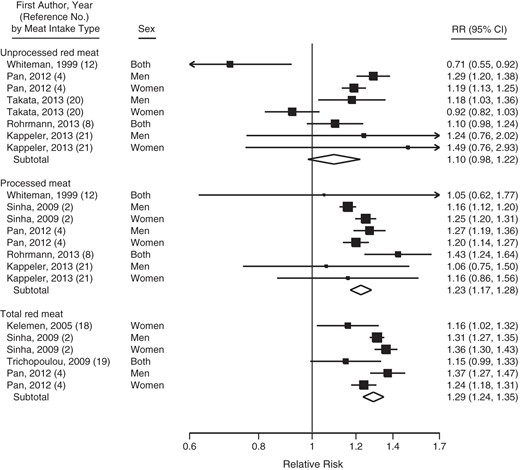
In meta-analysis combining the risk estimates for the highest versus the lowest category, consumption of processed meat and total red meat but not unprocessed red meat was statistically significantly positively associated with all-cause mortality (Figure 2). Although all relative risks for processed meat and total red meat consumption were greater than 1.0, there was statistically significant heterogeneity among study results (I2 ranged from 57% to 83%). We found no evidence of publication bias (P > 0.31).
Relative risk (RR) of all-cause mortality for the highest versus lowest category of unprocessed red meat, processed meat, and total red meat consumption. Squares represent study-specific relative risk estimates (size of the square reflects the study-specific statistical weight, i.e., the inverse of the variance); horizontal lines represent 95% confidence intervals (CIs); diamonds represent summary relative risks with 95% confidence intervals. Assessment of heterogeneity: unprocessed red meat, I2 = 83%, P < 0.001; processed meat, I2 = 57%; P = 0.022; total red meat, I2 = 65%; P = 0.014.
In analysis stratified by sex, processed meat consumption was associated with increased all-cause mortality in both men (relative risk (RR) = 1.20, 95% confidence interval (CI): 1.11, 1.30; Pheterogeneity = 0.05; n = 3 studies) and women (RR = 1.23, 95% CI: 1.19, 1.27; Pheterogeneity = 0.48; n = 3 studies). Likewise, total red meat consumption was positively associated with all-cause mortality in both men (RR = 1.32, 95% CI: 1.28, 1.37; Pheterogeneity = 0.27; n = 2 studies) and women (RR = 1.27, 95% CI: 1.17, 1.38; Pheterogeneity = 0.01; n = 3 studies). Unprocessed red meat consumption was positively associated with all-cause mortality in men (RR = 1.27, 95% CI: 1.19, 1.35; Pheterogeneity = 0.54; n = 3 studies) but not in women (RR = 1.09, 95% CI: 0.86, 1.37; Pheterogeneity < 0.001; n = 3 studies).
High consumption of processed meat was associated with increased all-cause mortality in studies conducted in the United States (RR = 1.21, 95% CI: 1.16, 1.26; Pheterogeneity = 0.07; n = 4 studies) and Europe (RR = 1.36, 95% CI: 1.10, 1.70; Pheterogeneity = 0.26; n = 2 studies). Similarly, total red meat consumption was positively associated with all-cause mortality both in studies from the United States (RR = 1.30, 95% CI: 1.25, 1.36; Pheterogeneity = 0.02; n = 4 studies) and Europe (RR = 1.15, 95% CI: 0.99, 1.33; n = 1 studies). Unprocessed red meat consumption was positively associated with all-cause mortality in studies from the United States (RR = 1.23, 95% CI: 1.17, 1.30; Pheterogeneity = 0.30; n = 3 studies) but not in European studies (RR = 0.90, 95% CI: 0.59, 1.38; Pheterogeneity = 0.002; n = 2 studies).
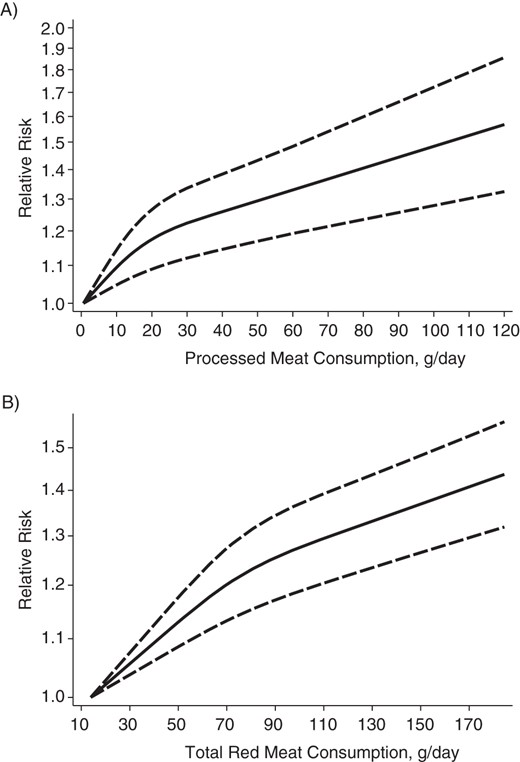
Dose-response meta-analysis
Three studies could not be included in the dose-response meta-analysis because red meat consumption was divided into 2 categories only (below and above the median) (19), confidence intervals were not provided for all categories (18), or the numbers of deaths and participants in each category were not reported (21). In a dose-response meta-analysis, consumption of processed meat (5 studies) and total red meat (3 studies) were significantly positively associated with all-cause mortality in a nonlinear fashion (Figure 3). The relative risk of all-cause mortality comparing 60 g/day (∼2 servings/day) with 10 g/day (∼2 servings/week) of processed meat consumption was 1.22 (95% CI: 1.13, 1.31). For total red meat consumption, the corresponding relative risk for 120 g/day (∼1.5 servings/day) versus 20 g/day (∼1.5–2 servings/week) was 1.29 (95% CI: 1.20, 1.38). Unprocessed red meat consumption (5 studies) showed a statistically nonsignificant linear association with all-cause mortality (for a 100-g/day increase in consumption, RR = 1.09, 95% CI: 0.997, 1.20).
Relative risks of all-cause mortality associated with A) processed meat, and B) total red meat consumption. Processed meat and total red meat consumption were modeled with restricted cubic splines in a random-effects dose-response model. A consumption of 0.6 g/day of processed meat (estimated median intake in the lowest exposure category) was used as the reference to estimate all relative risks for processed meat consumption. The corresponding reference for total red meat consumption was 13.9 g/day. The P values for nonlinearity were 0.003 for processed meat and less than 0.001 for total red meat consumption. The vertical axis is on a log scale.
DISCUSSION
Findings from this meta-analysis indicate that high consumption of red meat, in particular processed meat, is associated with higher all-cause mortality. Overall, those in the highest category of processed meat and total red meat consumption had increased all-cause mortality of 23% and 29%, respectively, compared with those in the lowest category. Unprocessed red meat consumption was not significantly associated with all-cause mortality. Results from the dose-response meta-analysis suggested that processed meat and total red meat consumption is associated with all-cause mortality in a nonlinear fashion with a steeper increase in all-cause mortality at intakes below approximately 1 serving per day. This finding suggests that all-cause mortality is elevated even at low intakes of processed meat and total red meat.
In a report by the World Cancer Research Fund (22), the public health recommendation with regard to cancer risk was to eat no more than 500 g (cooked weight) per week of red meat like beef, pork, and lamb and to avoid processed meats such as ham, bacon, salami, hot dogs, and sausages. Results from the present meta-analysis add to the increasing evidence that consumption of red meat, especially processed meat, should be limited.
Findings from the present meta-analysis are in agreement with previous meta-analyses on red meat and processed meat consumption in relationship to risk of chronic diseases. For example, a recent meta-analysis of 9 prospective studies found that the risk of type 2 diabetes increased by 19% for each 100-g/day increase of unprocessed red meat consumption and by 51% for each 50-g/day increase of processed meat consumption (1). In addition, summary results based on 5 prospective studies showed that the risk of coronary heart disease increased by 42% for each 50-g/day increment of processed meat consumption, whereas no association was observed between unprocessed red meat consumption and coronary heart disease (1). In another meta-analysis on stroke, each serving-per-day increase in unprocessed red meat or processed meat consumption was associated with 11% and 13% increased risks of stroke, respectively (3). Among cancer types, colorectal cancer has been most consistently associated with red meat and processed meat consumption (5, 7). One of the most recent meta-analyses showed that consumption of unprocessed red meat (100 g/day) and processed meat (50 g/day) was associated with 17% and 18% increased risks of colorectal cancer, respectively (7).
Red meat and processed meat consumption may increase all-cause mortality by increasing the risk of major chronic diseases, including cardiovascular disease and cancer. Processed meat usually contains much salt (sodium), which significantly raises blood pressure (23). In fact, red meat consumption has been associated with elevated blood pressure (24), which is a major cause of death worldwide (25). High salt intake may also promote vascular stiffness (23). Those with high consumption of red meat may consume fewer healthy foods such as fruits and vegetables, which are inversely associated with risk of cardiovascular disease (26, 27). In relationship to cancer, red meat is a source of carcinogens such as heterocyclic amines and polycyclic aromatic hydrocarbons, both of which are formed during the cooking of red meat at high temperatures (28). N-nitroso compounds, which are present in some processed meats and can be formed in a dose-dependent fashion related to the amount of red meat in the diet, may also increase cancer risk (28).
A limitation of this meta-analysis is the observational design of the included studies. Although most studies adjusted for major potential confounders such as smoking, physical activity, body mass index, and alcohol consumption, it cannot be ruled out that the observed association between red meat consumption and all-cause mortality is explained by residual confounding from, for example, socioeconomic status or other dietary factors such as fruit and vegetable consumption. Another limitation is that publication bias may have influenced the results. We could not detect any evidence of publication bias. However, tests for publication bias have low statistical power, especially when the number of studies is limited. Finally, although most studies indicated a positive association of processed meat and total meat consumption with all-cause mortality, there was significant heterogeneity among study results (different strength of associations). There are several potential explanations for the observed between-study heterogeneity. First, the range of meat consumption between the highest and lowest category, as well as the mean meat consumption in extreme categories, varied between studies. The risk estimates would be assumed to be higher in studies with broader ranges of red meat consumption. Second, the type of meat items included in the red meat and processed meat groups differed. Third, the length of follow-up varied from study to study with some studies having follow-up of more than 2 decades (4, 21). Nevertheless, 2 of the studies with long follow-up used repeated measurements of diet to account for changes in diet during follow-up and to reduce measurement error. Because the strength of the association of red meat consumption with all-cause mortality differed between studies, which resulted in statistical heterogeneity, the summary risk estimates should be interpreted with caution.
In conclusion, findings from this meta-analysis showed a positive association between the consumption of red meat, particularly processed meat, and all-cause mortality. These results add to and extend the evidence that high red meat consumption may have adverse health consequences.
ACKNOWLEDGMENTS
Author affiliations: Unit of Nutritional Epidemiology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden (Susanna C. Larsson, Nicola Orsini).
This work was supported by research grants from the Swedish Research Council for Health, Working Life and Welfare (Forte).
The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Conflict of interest: none declared.
REFERENCES
Author notes
Abbreviations: CI, confidence interval; RR, relative risk.